What you need to know about research dissemination
Last updated
5 March 2024
Reviewed by
Short on time? Get an AI generated summary of this article instead
In this article, we'll tell you what you need to know about research dissemination.
- Understanding research dissemination
Research that never gets shared has limited benefits. Research dissemination involves sharing research findings with the relevant audiences so the research’s impact and utility can reach its full potential.
When done effectively, dissemination gets the research into the hands of those it can most positively impact. This may include:
Politicians
Industry professionals
The general public
What it takes to effectively disseminate research will depend greatly on the audience the research is intended for. When planning for research dissemination, it pays to understand some guiding principles and best practices so the right audience can be targeted in the most effective way.
- Core principles of effective dissemination
Effective dissemination of research findings requires careful planning. Before planning can begin, researchers must think about the core principles of research dissemination and how their research and its goals fit into those constructs.
Research dissemination principles can best be described using the 3 Ps of research dissemination.
This pillar of research dissemination is about clarifying the objective. What is the goal of disseminating the information? Is the research meant to:
Persuade policymakers?
Influence public opinion?
Support strategic business decisions?
Contribute to academic discourse?
Knowing the purpose of sharing the information makes it easy to accurately target it and align the language used with the target audience .
The process includes the methods that will be used and the steps taken when it comes time to disseminate the findings. This includes the channels by which the information will be shared, the format it will be shared in, and the timing of the dissemination.
By planning out the process and taking the time to understand the process, researchers will be better prepared and more flexible should changes arise.
The target audience is whom the research is aimed at. Because different audiences require different approaches and language styles, identifying the correct audience is a huge factor in the successful dissemination of findings.
By tailoring the research dissemination to the needs and preferences of a specific audience, researchers increase the chances of the information being received, understood, and used.
- Types of research dissemination
There are many options for researchers to get their findings out to the world. The type of desired dissemination plays a big role in choosing the medium and the tone to take when sharing the information.
Some common types include:
Academic dissemination: Sharing research findings in academic journals, which typically involves a peer-review process.
Policy-oriented dissemination: Creating documents that summarize research findings in a way that's understandable to policymakers.
Public dissemination: Using television and other media outlets to communicate research findings to the public.
Educational dissemination: Developing curricula for education settings that incorporate research findings.
Digital and online dissemination: Using digital platforms to present research findings to a global audience.
Strategic business presentation: Creating a presentation for a business group to use research insights to shape business strategy
- Major components of information dissemination
While the three Ps provide a convenient overview of what needs to be considered when planning research dissemination, they are not a complete picture.
Here’s a more comprehensive list of what goes into the dissemination of research results:
Audience analysis : Identifying the target audience and researching their needs, preferences, and knowledge level so content can be tailored to them.
Content development: Creating the content in a way that accurately reflects the findings and presents them in a way that is relevant to the target audience.
Channel selection: Choosing the channel or channels through which the research will be disseminated and ensuring they align with the preferences and needs of the target audience.
Timing and scheduling: Evaluating factors such as current events, publication schedules, and project milestones to develop a timeline for the dissemination of the findings.
Resource allocation: With the basics mapped out, financial, human, and technological resources can be set aside for the project to facilitate the dissemination process.
Impact assessment and feedback: During the dissemination, methods should be in place to measure how successful the strategy has been in disseminating the information.
Ethical considerations and compliance: Research findings often include sensitive or confidential information. Any legal and ethical guidelines should be followed.
- Crafting a dissemination blueprint
With the three Ps providing a foundation and the components outlined above giving structure to the dissemination, researchers can then dive deeper into the important steps in crafting an impactful and informative presentation.
Let’s take a look at the core steps.

1. Identify your audience
To identify the right audience for research dissemination, researchers must gather as much detail as possible about the different target audience segments.
By gathering detailed information about the preferences, personalities, and information-consumption habits of the target audience, researchers can craft messages that resonate effectively.
As a simple example, academic findings might be highly detailed for scholarly journals and simplified for the general public. Further refinements can be made based on the cultural, educational, and professional background of the target audience.
2. Create the content
Creating compelling content is at the heart of effective research dissemination. Researchers must distill complex findings into a format that's engaging and easy to understand. In addition to the format of the presentation and the language used, content includes the visual or interactive elements that will make up the supporting materials.
Depending on the target audience, this may include complex technical jargon and charts or a more narrative approach with approachable infographics. For non-specialist audiences, the challenge is to provide the required information in a way that's engaging for the layperson.
3. Take a strategic approach to dissemination
There's no single best solution for all research dissemination needs. What’s more, technology and how target audiences interact with it is constantly changing. Developing a strategic approach to sharing research findings requires exploring the various methods and channels that align with the audience's preferences.
Each channel has a unique reach and impact, and a particular set of best practices to get the most out of it. Researchers looking to have the biggest impact should carefully weigh up the strengths and weaknesses of the channels they've decided upon and craft a strategy that best uses that knowledge.
4. Manage the timeline and resources
Time constraints are an inevitable part of research dissemination. Deadlines for publications can be months apart, conferences may only happen once a year, etc. Any avenue used to disseminate the research must be carefully planned around to avoid missed opportunities.
In addition to properly planning and allocating time, there are other resources to consider. The appropriate number of people must be assigned to work on the project, and they must be given adequate financial and technological resources. To best manage these resources, regular reviews and adjustments should be made.
- Tailoring communication of research findings
We’ve already mentioned the importance of tailoring a message to a specific audience. Here are some examples of how to reach some of the most common target audiences of research dissemination.
Making formal presentations
Content should always be professional, well-structured, and supported by data and visuals when making formal presentations. The depth of information provided should match the expertise of the audience, explaining key findings and implications in a way they'll understand. To be persuasive, a clear narrative and confident delivery are required.
Communication with stakeholders
Stakeholders often don't have the same level of expertise that more direct peers do. The content should strike a balance between providing technical accuracy and being accessible enough for everyone. Time should be taken to understand the interests and concerns of the stakeholders and align the message accordingly.
Engaging with the public
Members of the public will have the lowest level of expertise. Not everyone in the public will have a technical enough background to understand the finer points of your message. Try to minimize confusion by using relatable examples and avoiding any jargon. Visual aids are important, as they can help the audience to better understand a topic.
- 10 commandments for impactful research dissemination
In addition to the details above, there are a few tips that researchers can keep in mind to boost the effectiveness of dissemination:
Master the three Ps to ensure clarity, focus, and coherence in your presentation.
Establish and maintain a public profile for all the researchers involved.
When possible, encourage active participation and feedback from the audience.
Use real-time platforms to enable communication and feedback from viewers.
Leverage open-access platforms to reach as many people as possible.
Make use of visual aids and infographics to share information effectively.
Take into account the cultural diversity of your audience.
Rather than considering only one dissemination medium, consider the best tool for a particular job, given the audience and research to be delivered.
Continually assess and refine your dissemination strategies as you gain more experience.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 24 October 2024
Last updated: 30 January 2024
Last updated: 11 January 2024
Last updated: 17 January 2024
Last updated: 12 December 2023
Last updated: 30 April 2024
Last updated: 4 July 2024
Last updated: 12 October 2023
Last updated: 5 March 2024
Last updated: 31 January 2024
Last updated: 23 January 2024
Last updated: 13 May 2024
Last updated: 20 December 2023
Latest articles
Related topics, a whole new way to understand your customer is here, log in or sign up.
Get started for free
Loading metrics
Open Access
Ten simple rules for innovative dissemination of research
* E-mail: [email protected]
Affiliation Open and Reproducible Research Group, Institute of Interactive Systems and Data Science, Graz University of Technology and Know-Center GmbH, Graz, Austria
Affiliation Center for Research and Interdisciplinarity, University of Paris, Paris, France
Affiliation Freelance Researcher, Vilnius, Lithuania
Affiliation University and National Library, University of Debrecen, Debrecen, Hungary
Affiliation Institute for Research on Population and Social Policies, National Research Council, Rome, Italy
Affiliation Open Knowledge Maps, Vienna, Austria
Affiliation National and Kapodistrian University of Athens, Athens, Greece
Affiliation Center for Digital Safety and Security, AIT Austrian Institute of Technology, Vienna, Austria
- Tony Ross-Hellauer,
- Jonathan P. Tennant,
- Viltė Banelytė,
- Edit Gorogh,
- Daniela Luzi,
- Peter Kraker,
- Lucio Pisacane,
- Roberta Ruggieri,
- Electra Sifacaki,
- Michela Vignoli

Published: April 16, 2020
- https://doi.org/10.1371/journal.pcbi.1007704
- Reader Comments
Author summary
How we communicate research is changing because of new (especially digital) possibilities. This article sets out 10 easy steps researchers can take to disseminate their work in novel and engaging ways, and hence increase the impact of their research on science and society.
Citation: Ross-Hellauer T, Tennant JP, Banelytė V, Gorogh E, Luzi D, Kraker P, et al. (2020) Ten simple rules for innovative dissemination of research. PLoS Comput Biol 16(4): e1007704. https://doi.org/10.1371/journal.pcbi.1007704
Editor: Russell Schwartz, Carnegie Mellon University, UNITED STATES
Copyright: © 2020 Ross-Hellauer et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This work was partly funded by the OpenUP project, which received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 710722. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: We have read the journal's policy and have the following conflicts: TR-H is Editor-in-Chief of the open access journal Publications . JT is the founder of the Open Science MOOC, and a former employee of ScienceOpen.
Introduction
As with virtually all areas of life, research dissemination has been disrupted by the internet and digitally networked technologies. The last two decades have seen the majority of scholarly journals move online, and scholarly books are increasingly found online as well as in print. However, these traditional communication vehicles have largely retained similar functions and formats during this transition. But digital dissemination can happen in a variety of ways beyond the traditional modes: social media have become more widely used among researchers [ 1 , 2 , 3 ], and the use of blogs and wikis as a specific form of ‘open notebook science’ has been popular for more than a decade [ 4 ].
Professional academic social networks such as ResearchGate and Academia.edu boast millions of users. New online formats for interaction with the wider public, such as TED talks broadcast via YouTube, often receive millions of views. Some researchers have even decided to make all of their research findings public in real time by keeping open notebooks [ 5 , 6 ]. In particular, digital technologies invoke new ways of reaching and involving audiences beyond their usual primary dissemination targets (i.e., other scholars) to actively involve peers or citizens who would otherwise remain out of reach for traditional methods of communication [ 7 ]. Adoption of these outlets and methods can also lead to new cross-disciplinary collaborations, helping to create new research, publication, and funding opportunities [ 8 ].
Beyond the increase in the use of web-based and computational technologies, other trends in research cultures have had a profound effect on dissemination. The push towards greater public understanding of science and research since the 1980s, and an emphasis on engagement and participation of non-research audiences have brought about new forms of dissemination [ 9 ]. These approaches include popular science magazines and science shows on television and the radio. In recent years, new types of events have emerged that aim at involving the general public within the research process itself, including science slams and open lab days. With science cafés and hackerspaces, novel, participatory spaces for research production and dissemination are emerging—both online and offline. Powerful trends towards responsible research and innovation, the increasing globalisation of research, and the emergence and inclusion of new or previously excluded stakeholders or communities are also reshaping the purposes of dissemination as well as the scope and nature of its audiences.
Many now view wider dissemination and public engagement with science to be a fundamental element of open science [ 10 ]. However, there is a paradox at play here, for while there have never been more avenues for the widespread dissemination of research, researchers tend nonetheless to value and focus upon just a few traditional outputs: journal articles, books, and conference presentations [ 11 ].
Following Wilson and colleagues [ 12 ], we here define research dissemination as a planned process that involves consideration of target audiences, consideration of the settings in which research findings are to be received, and communicating and interacting with wider audiences in ways that will facilitate research uptake and understanding. Innovative dissemination, then, means dissemination that goes beyond traditional academic publishing (e.g., academic journals, books, or monographs) and meetings (conferences and workshops) to achieve more widespread research uptake and understanding. Hence, a citizen science project, which involves citizens in data collection but does not otherwise educate them about the research, is not here considered innovative dissemination.
We here present 10 steps researchers can take to embrace innovative dissemination practices in their research, either as individuals or groups ( Fig 1 ). They represent the synthesis of multidimensional research activities undertaken within the OpenUP project ( https://www.openuphub.eu/ ). This European Coordination and Support Action grant award addressed key aspects and challenges of the currently transforming science landscape and proposed recommendations and solutions addressing the needs of researchers, innovators, the public, and funding bodies. The goal is to provide stakeholders (primarily researchers but also intermediaries) with an entry point to innovative dissemination, so that they can choose methods and tools based on their audience, their skills, and their requirements. The advice is directed towards both individual researchers and research teams or projects. It is similar to other entries in the Ten Simple Rules series (e.g., [ 13 , 14 ]). Ultimately, the benefit here for researchers is increased recognition and social impact of their work.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pcbi.1007704.g001
Rule 1: Get the basics right
Despite changes in communication technologies and models, there are some basic organisational aspects of dissemination that remain important: to define objectives, map potential target audience(s), target messages, define mode of communication/engagement, and create a dissemination plan. These might seem a bit obvious or laborious but are critical first steps towards strategically planning a project.
Define objectives
The motivation to disseminate research can come in many forms. You might want to share your findings with wider nonacademic audiences to raise awareness of particular issues or invite audience engagement, participation, and feedback. Start by asking yourself what you want to achieve with your dissemination. This first strategic step will make all other subsequent steps much simpler, as well as guide how you define the success of your activities.
Map your audience
Specify who exactly you want your research results to reach, for which purposes, and what their general characteristics might be (e.g., policy makers, patient groups, non-governmental organisations). Individuals are not just ‘empty vessels’ to be filled with new knowledge, and having a deeper contextual understanding of your audience can make a real difference to the success of your engagement practices. Who is most affected by your research? Who might find it most valuable? What is it that you want them to take away? Get to know your target audiences, their needs and expectations of the research outcomes, as well as their preferred communication channels to develop a detailed understanding of their interests and align your messages and media with their needs and priorities. Keep in mind, too, that intermediaries such as journalists or science communication organisations can support or mediate the dissemination process.
Target/frame your messages
Target and frame the key messages that you want to communicate to specific groups. Think first from the perspective of what they might want or need to hear from you, rather than what you want to tell them. Choosing media and format of your communication strongly depends on your communication objectives, i.e., what you want to achieve. There are many ways to communicate your research; for example, direct messages, blog/vlog posts, tweeting about it, or putting your research on Instagram. Form and content go hand in hand. Engage intermediaries and leverage any relevant existing networks to help amplify messages.
Create a dissemination plan
Many funded research projects require a dissemination plan. However, even if not, the formal exercise of creating a plan at the outset that organises dissemination around distinct milestones in the research life cycle will help you to assign roles, structure activities, as well as plan funds to be allocated in your dissemination. This will ultimately save you time and make future work easier. If working in groups, distribute tasks and effort to ensure regular updates of content targeted to different communities. Engage those with special specific skills in the use and/or development of appropriate communication tools, to help you in using the right language and support you in finding the suitable occasions to reach your identified audience. Research is not linear, however, and so you might find it best to treat the plan as a living document to be flexibly adapted as the direction of research changes.
Rule 2: Keep the right profile
Whether communicating as an individual researcher, a research project, or a research organisation, establishing a prominent and unique identity online and offline is essential for communicating. Use personal websites, social media accounts, researcher identifiers, and academic social networks to help make you and your research visible. When doing this, try to avoid any explicit self-promotion—your personal profile naturally will develop based on your ability to be an effective and impactful communicator.
Academia is a prestige economy, where individual researchers are often evaluated based on their perceived esteem or standing within their communities [ 15 ]. Remaining visible is an essential part of accumulating esteem. An online presence maintained via personal websites, social media accounts (e.g., Facebook, Twitter, LinkedIn), researcher identifiers (e.g., ORCID), and academic social networks (e.g., ResearchGate, institutional researcher profiles) can be a personal calling card, where you can highlight experience and demonstrate your expertise in certain topics. Being active on important mailing lists, forums, and social media is not only a good chance to disseminate your findings to those communities but also offers you the chance to engage with your community and potentially spark new ideas and collaborations.
Using researcher identifiers like ORCID when disseminating outputs will ensure that those outputs will be unambiguously linked back to the individual researcher (and even automatically updated to their ORCID profile). The OpenUP survey showed that nearly half of the respondents (41%) use academic social networks as a medium to disseminate their research, and a quarter of respondents (26%) said that these networks informed their professional work [ 16 ].
Create a brand by giving your project a unique name, ideally with some intuitive relation to the issue you are investigating. Create a striking visual identity, with a compelling logo, core colours, and a project slogan. Create a website that leverages this visual identity and is as simple and intuitive as possible, both in its layout and in the way content is formulated (limit insider jargon). Create associated appropriate social media accounts (e.g., Twitter, Facebook, LinkedIn, SlideShare, YouTube) and link to this from the project website. Aim for a sustained presence with new and engaging content to reinforce project messaging, and this can help to establish a core following group or user base within different platforms. Include links to other project online presences such as social media accounts, or a rolling feed of updates if possible. Consider including a blog to disseminate core findings or give important project updates. A periodical newsletter could be released in order to provide project updates and other news, to keep the community informed and activated regarding project issues. Depending on the size of your project and budget, you might want to produce hard copy material such as leaflets or fact sheets, as well as branded giveaways to increase awareness of your project. Finally, and perhaps most importantly, try not to come across as a ‘scientific robot’, and make sure to communicate the more human personality side of research.
Rule 3: Encourage participation
In the age of open research, don’t just broadcast. Invite and engage others to foster participation and collaboration with research audiences. Scholarship is a collective endeavour, and so we should not expect its dissemination to be unidirectional, especially not in the digital age. Dissemination is increasingly done at earlier stages of the research life cycle, and such wider and more interactive engagement is becoming an integral part of the whole research workflow.
Such participative activities can be as creative as you wish; for example, through games, such as Foldit for protein folding ( https://fold.it/portal/ ). You might even find it useful to actively engage ‘citizen scientists’ in research projects; for example, to collect data or analyse findings. Initiatives such as Zooniverse ( https://www.zooniverse.org/ ) serve as great examples of allowing anyone to freely participate in cutting-edge ‘people-powered research’.
Disseminating early and often showcases the progress of your work and demonstrates productivity and engagement as part of an agile development workflow. People like to see progress and react positively to narrative, so give regular updates to followers on social media, for example, blogging or tweeting early research findings for early feedback. Alternatively, involving businesses early on can align research to industry requirements and expectations, thus potentially increasing commercial impact. In any case, active involvement of citizens and other target audiences beyond academia can help increase the societal impact of your research [ 17 ].
Rule 4: Open science for impact
Open science is ‘transparent and accessible knowledge that is shared and developed through collaborative networks’, as defined by one systematic review [ 18 ]. It encompasses a variety of practices covering a range of research processes and outputs, including areas like open access (OA) to publications, open research data, open source software/tools, open workflows, citizen science, open educational resources, and alternative methods for research evaluation including open peer review [ 19 ]. Open science is rooted in principles of equitable participation and transparency, enabling others to collaborate in, contribute to, scrutinise and reuse research, and spread knowledge as widely as possible [ 20 ]. As such, innovative dissemination is a core element of open science.
Embracing open science principles can boost the impact of research. Firstly, OA publications seem to accrue more citations than their closed counterparts, as well as having a variety of possible wider economic and societal benefits [ 21 ]. There are a number of ways to make research papers OA, including at the journal site itself, or self-archiving an accepted manuscript in a repository or personal website.
Disseminating publications as preprints in advance of or parallel to journal submission can increase impact, as measured by relative citation counts [ 22 ]. Very often, traditional publishing takes a long time, with the waiting time between submission and acceptance of a paper being in excess of 100 days [ 23 ]. Preprinting speeds up dissemination, meaning that findings are available sooner for sharing and reuse. Potential platforms for disseminating preprints include the Open Science Framework, biorXiv, or arXiv.
Dissemination of other open science outputs that would usually remain hidden also not only helps to ensure the transparency and increased reproducibility of research [ 24 ], but also means that more research elements are released that can potentially impact upon others by creating network effects through reuse. Making FAIR (Findable, Accessible, Interoperable, Reusable) research data and code available enables reuse and remixing of core research outputs, which can also lead to further citations for projects [ 25 , 26 , 27 ]. Published research proposals, protocols, and open notebooks act as advertisements for ongoing research and enable others to reuse methods, exposing the continuous and collaborative nature of scholarship.
To enable reuse, embrace open licenses. When it comes to innovative dissemination, the goal is usually that the materials are accessible to as large an audience as possible. If appropriate open licenses are not used, while materials may be free to access, they cannot be widely used, modified, or shared. The best in this case is the widely adopted Creative Commons licenses, CC BY or CC 0. Variations of these licenses are less permissive and can constrain reuse for commercial or derivative purposes. This limitation, however, prevents the use of materials in many forms of (open) educational resources and other open projects, including Wikipedia. Careful consideration should be given to licensing of materials, depending on what your intended outcomes from the project are (see Rule 1). Research institutes and funding bodies typically have a variety of policies and guidance about the use and licensing of such materials, and should be consulted prior to releasing any materials.
Rule 5: Remix traditional outputs
Traditional research outputs like research articles and books can be complemented with innovative dissemination to boost impact; for example, by preparing accompanying nonspecialist summaries, press releases, blog posts, and visual/video abstracts to better reach your target audiences. Free media coverage can be an easy way to get results out to as many people as possible. There are countless media outlets interested in science-related stories. Most universities and large research organisations have an office for public affairs or communication: liaise with these experts to disseminate research findings widely through public media. Consider writing a press release for manuscripts that have been accepted for publication in journals or books and use sample forms and tools available online to assist you in the process. Some journals also have dedicated press teams that might be able to help you with this.
Another useful tool to disseminate traditional research outputs is to release a research summary document. This one- or two-page document clearly and concisely summarises the key conclusions from a research initiative. It can combine several studies by the same investigator or by a research group and should integrate two main components: key findings and fact sheets (preferably with graphical images to illustrate your point). This can be published on your institutional website as well as on research blogs, thematic hubs, or simply posted on your social media profiles. Other platforms such as ScienceOpen and Kudos allow authors to attach nonspecialist summaries to each of their research papers.
To maximise the impact of your conference presentations or posters, there are several steps that can be taken. For instance, you can upload your slides to a general-purpose repository such as Figshare or Zenodo and add a digital object identifier (DOI) to your presentation. This also makes it easier to integrate such outputs with other services like ORCID. You can also schedule tweets before and during any conferences, and use the conference hashtag to publicise your talk or poster. Finally, you can also add information about your contributions to email signatures or out-of-office messages [ 28 ].
Rule 6: Go live
In-person dissemination does not just have to be at stuffy conferences. With research moving beyond the walls of universities, there are several types of places for more participatory events. Next to classic scientific conferences, different types of events addressing wider audiences have emerged. It is possible to hit the road and take part in science festivals, science slams, TEDx talks, or road shows.
Science slams are short talks in which researchers explain a scientific topic to a typically nonexpert audience. Similar to other short talk formats like TED talks, they lend themselves to being spread over YouTube and other video channels. A prominent example from the German-speaking area is Giulia Enders, who won the first prize in a science slam that took place in 2012 in Berlin. The YouTube video of her fascinating talk about the gut has received over 1 million views. After this success, she got an offer to write a book about the gut and the digestive system, which has since been published and translated into many languages. You never know how these small steps might end up having a wider impact on your research and career.
Another example is Science Shops, small entities which provide independent, participatory research support to civil society. While they are usually linked to universities, hacker and maker spaces tend to be community-run locations, where people with an interest in science, engineering, and art meet and collaborate on projects. Science festivals are community-based showcases of science and technology that take place over large areas for several days or weeks and directly involve researchers and practitioners in public outreach. Less formally, Science Cafés or similar events like Pint of Science are public engagement events in casual settings like pubs and coffeehouses.
Alternatively, for a more personal approach, consider reaching out to key stakeholders who might be affected by your research and requesting a meeting, or participating in relevant calls for policy consultations. Such an approach can be especially powerful in getting the message across to decision-makers and thought-leaders, although the resources required to schedule and potentially travel to such meetings means you should target such activities very carefully. And don’t forget the value of serendipity—who knows who you’ll meet in the course of your everyday meetings and travels. Always be prepared with a 30 second ‘elevator pitch’ that sums up your project in a confident and concise manner—such encounters may be the gateways to greater engagement or opportunities.
Rule 7: Think visual
Dissemination of research is still largely ruled by the written or spoken word. However, there are many ways to introduce visual elements that can act as attractive means to help your audience understand and interpret your research. Disseminate findings through art or multimedia interpretations. Let your artistic side loose or use new visualisation techniques to produce intuitive, attractive data displays. Of course, not everyone is a trained artist, and this will be dependent on your personal skills.
Most obviously, this could take the form of data visualisation. Graphic representation of quantitative information reaches back to ‘earliest map-making and visual depiction’ [ 29 ]. As technologies have advanced, so have our means of visually representing data.
If your data visualisations could be considered too technical and not easily understandable by a nonexpert reader, consider creating an ad hoc image for this document; sometimes this can also take the form of a graphical abstract or infographic. Use online tools to upload a sample of your data and develop smart graphs and infographics (e.g., Infogr.am, Datawrapper, Easel.ly, or Venngage).
Science comics can be used, in the words of McDermott, Partridge, and Bromberg [ 30 ], to ‘communicate difficult ideas efficiently, illuminate obscure concepts, and create a metaphor that can be much more memorable than a straightforward description of the concept itself’. McDermott and colleagues continue that comics can be used to punctuate or introduce papers or presentations and to capture and share the content of conference talks, and that some journals even have a ‘cartoon’ publication category. They advise that such content has a high chance of being ‘virally’ spread via social media.
As previously discussed, you may also consider creating a video abstract for a paper or project. However, as with all possible methods, it is worth considering the relative costs versus benefits of such an approach. Creating a high-quality video might have more impact than, say, a blog post but could be more costly to produce.
Projects have even successfully disseminated scientific findings through art. For example, The Civilians—a New York–based investigative theatre company—received a three-year grant to develop The Great Immensity , a play addressing the complexity of climate change. AstroDance tells the story of the search for gravitational waves through a combination of dance, multimedia, sound, and computer simulations. The annual Dance Your PhD contest, which began in 2007 and is sponsored by Science magazine, even asks scientists to interpret their PhD research as dance. This initiative receives approximately 50 submissions a year, demonstrating the popularity of novel forms of research dissemination.
Rule 8: Respect diversity
The academic discourse on diversity has always included discussions on gender, ethnic and cultural backgrounds, digital literacy, and epistemic, ideological, or economic diversity. An approach that is often taken is to include as many diverse groups into research teams as possible; for example, more women, underrepresented minorities, or persons from developing countries. In terms of scientific communication, however, not only raising awareness about diversity issues but also increasing visibility of underrepresented minorities in research or including more women in science communication teams should be considered, and embedded in projects from the outset. Another important aspect is assessing how the communication messages are framed, and if the chosen format and content is appropriate to address and respect all audiences. Research should reach all who might be affected by it. Respect inclusion in scientific dissemination by creating messages that reflect and respect diversity regarding factors like gender, demography, and ability. Overcoming geographic barriers is also important, as well as the consideration of differences in time zones and the other commitments that participants might have. As part of this, it is a key responsibility to create a healthy and welcoming environment for participation. Having things such as a code of conduct, diversity statement, and contributing guidelines can really help provide this for projects.
The 2017 Progression Framework benchmarking report of the Scientific Council made several recommendations on how to make progress on diversity and inclusion in science: (1) A strategy and action plan for diversity should developed that requires action from all members included and (2) diversity should be included in a wide range of scientific activities, such as building diversity into prizes, awards, or creating guidance on building diversity and inclusion across a range of demographics groups into communications, and building diversity and inclusion into education and training.
Rule 9: Find the right tools
Innovative dissemination practices often require different resources and skills than traditional dissemination methods. As a result of different skills and tools needed, there may be higher costs associated with some aspects of innovative dissemination. You can find tools via a more-complete range of sources, including the OpenUP Hub. The Hub lists a catalogue of innovative dissemination services, organised according to the following categories, with some suggested tools:
- Visualising data: tools to help create innovative visual representations of data (e.g., Nodegoat, DataHero, Plot.ly)
- Sharing notebooks, protocols, and workflows: ways to share outputs that document and share research processes, including notebooks, protocols, and workflows (e.g., HiveBench, Protocols.io, Open Notebook Science Network)
- Crowdsourcing and collaboration: platforms that help researchers and those outside academia to come together to perform research and share ideas (e.g., Thinklab, Linknovate, Just One Giant Lab)
- Profiles and networking: platforms to raise academic profile and find collaboration and funding opportunities with new partners (e.g., Humanities Commons, ORCID, ImpactStory)
- Organiding events: tools to help plan, facilitate, and publicise academic events (e.g., Open Conference Systems, Sched, ConfTool)
- Outreach to wider public: channels to help broadcast your research to audiences beyond academia, including policy makers, young people, industry, and broader society (e.g., Famelab, Kudos, Pint of Science)
- Publishing: platforms, tools, and services to help you publish your research (e.g., Open Science Framework, dokieli, ScienceMatters)
- Archive and share: preprint servers and repositories to help you archive and share your texts, data, software, posters, and more (e.g., BitBucket, GitHub, RunMyCode)
The Hub here represents just one attempt to create a registry of resources related to scholarly communication. A similar project is the 101 Innovations in Scholarly Communication project, which contains different tools and services for all parts of a generalised research workflow, including dissemination and outreach. This can be broadly broken down into services for communication through social media (e.g., Twitter), as well as those designed for sharing of scholarly outputs, including posters and presentations (e.g., Zenodo or Figshare). The Open Science MOOC has also curated a list of resources for its module on Public Engagement with Science, and includes key research articles, organisations, and services to help with wider scientific engagement.
Rule 10: Evaluate, evaluate, evaluate
Assess your dissemination activities. Are they having the right impact? If not, why not? Evaluation of dissemination efforts is an essential part of the process. In order to know what worked and which strategies did not generate the desired outcomes, all the research activities should be rigorously assessed. Such evaluation should be measured via the use of a combination of quantitative and qualitative indicators (which should be already foreseen in the planning stage of dissemination; see Rule 1). Questionnaires, interviews, observations, and assessments could also be used to measure the impact. Assessing and identifying the most successful practices will give you the evidence for the most effective strategies to reach your audience. In addition, the evaluation can help you plan your further budget and minimise the spending and dedicating efforts on ineffective dissemination methods.
Some examples of quantitative indicators include the following:
- Citations of publications;
- alternative metrics related to websites and social media platforms (updates, visits, interactions, likes, and reposts);
- numbers of events held for specific audiences;
- numbers of participants in those events;
- production and circulation of printed materials;
- media coverage (articles in specialised press newsletters, press releases, interviews, etc.); and
- how much time and effort were spent on activities.
Some examples of qualitative indicators include the following:
- Visibility in the social media and attractiveness of website;
- newly established contacts with networks and partners and the outcomes of these contacts;
- feedback from the target groups; and
- share feedback within your group on what dissemination strategies seemed to be the most effective in conveying your messages and reaching your target audiences.
We recognise that researchers are usually already very busy, and we do not seek to pressurise them further by increasing their burdens. Our recommendations, however, come at a time when there are shifting norms in how researchers are expected to engage with society through new technologies. Researchers are now often partially evaluated based on such, or expected to include dissemination plans in grant applications. We also do not want to encourage the further fragmentation of scholarship across different platforms and ‘silos’, and therefore we strongly encourage researchers to be highly strategic in how they engage with different methods of innovative dissemination. We hope that these simple rules provide guidance for researchers and their future projects, especially as the tools and services available evolve through time. Some of these suggestions or platforms might not work across all project types, and it is important for researchers to find which methods work best for them.
Acknowledgments
Many thanks to everyone who engaged with the workshops we conducted as part of this grant award.
- View Article
- Google Scholar
- PubMed/NCBI
- 19. Pontika N, Knoth P, Cancellieri M, Pearce S. Fostering Open Science to Research Using a Taxonomy and an ELearning Portal. In: iKnow: 15th International Conference on Knowledge Technologies and Data Driven Business, 21–22 Oct 2015, Graz, Austria [cited 2020 Mar 23]. Available from: http://oro.open.ac.uk/44719/
- 29. Friendly M. A Brief History of Data Visualization. In: Handbook of Data Visualization . Chen C, Härdle W, Unwin A, editors. Springer Handbooks Comp.Statistics. Berlin, Heidelberg: Springer Berlin Heidelberg. https://doi.org/10.1007/978-3-540-33037-0_2 . 2008. Pp.15–56.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 28, Issue 3
- Responsible dissemination of health and medical research: some guidance points
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-7765-2443 Raffaella Ravinetto 1 ,
- http://orcid.org/0000-0002-6275-6853 Jerome Amir Singh 2 , 3
- 1 Public Health Department , Institute of Tropical Medicine , Antwerpen , Belgium
- 2 Howard College School of Law , University of Kwazulu-Natal , Durban , South Africa
- 3 Dalla Lana School of Public Health , University of Toronto , Toronto , Ontario , Canada
- Correspondence to Dr Raffaella Ravinetto, Public Health Department, Institute of Tropical Medicine, Antwerpen, Belgium; rravinetto{at}itg.be
https://doi.org/10.1136/bmjebm-2022-111967
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- PUBLIC HEALTH
- Global Health
Ravinetto and Singh argue that better practices can be implemented when disseminating research findings through abstracts, preprints, peer-reviewed publications, press releases and social media
Dissemination has been defined as ‘the targeted distribution of information and intervention materials to a specific public health or clinical practice audience’, 1 and as being ‘simply about getting the findings of your research to the people who can make use of them, to maximise the benefit of the research without delay’. 2 Ethics guidelines concur that research stakeholders have ethical obligations to disseminate positive, inconclusive or negative results, 3 in an accurate, comprehensive and transparent way 4 —even more so during public health emergencies. 5
Summary of research dissemination
What —Dissemination of health and medical research entails communicating the findings of research to stakeholders in ways that can facilitate understanding and use.
Why —Any positive, inconclusive or negative research findings should be disseminated to maximise the social value of the research and to accurately inform medical policies and practices.
When —Dissemination of health and medical research should occur as soon as possible after completion of interim and final analysis, particularly during public health emergencies.
Who —Researchers, research institutions, sponsors, developers, publishers and editors must ensure the timely and accurate dissemination of research findings. Similarly, the scientific community should critically appraise research findings; policymakers and clinicians should weigh the implications of research findings for policy and clinical practice; while mainstream media should communicate the implications of research findings to the general public in a manner that facilitates understanding.
How —Research findings are primarily disseminated via press releases, preprints, abstracts and peer-reviewed publications. To ensure timely, comprehensive, accurate, unbiased, unambiguous and transparent dissemination, all research stakeholders should integrate ethics and integrity principles in their institutional dissemination policies and personal belief systems.
Peer-reviewed publications
Publication in peer-reviewed journals remains the benchmark dissemination modality. Independent peer-review aims to assure the quality, accuracy and credibility of reports, but does not always prevent the publication of poorly written, dubious or even fraudulent manuscripts, 9 particularly if there is dearth of qualified reviewers, and/or an findings are hastily published to gain competitive advantage and visibility. 10 Furthermore, researchers who are inexperienced or subject to an institutional ethos of ‘publish or perish’, may choose to publish in predatory journals with highly questionable marketing and peer-review practices. 11 While target audiences may be unable to access findings if journal content is not freely accessible on the Internet, some researchers, particularly those in resource-constrained settings 12 may be unable to publish their research due to resource constraints (eg, publication fees may be prohibitively high). 13 Some may be poorly motivated to publish inconclusive or negative data. 14 Because of such shortcomings, commentators such as Horby warn that ‘clinicians should not rely solely on peer review to assess the validity and meaningfulness of research findings’. 15
For peer-reviewed publications to remain a key-dissemination modality, editors should follow the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals , of the International Committee of Medical Journal Editors, and comply with the core practices of the Committee on Publication Ethics (eg, data and reproducibility, ethical oversight, authorship and contributorship, etc.). This entails going beyond a ‘checklist approach’ and subjecting manuscripts to rigorous screening and assessment. Journals should strive to select qualified independent reviewers and prioritise open-access policies. Research institutions should distance themselves from a ‘publish or perish’ culture which, together with the willingness to hide ‘unfavourable’ results, remains a major driver of unethical publication practices—which, in turn, translates to ill-informed policies and practices. 16
Scientific conferences are valuable venues for sharing research results with peers, and getting prepublication critical feedback. Abstracts often appear in the supplement of a scientific journal, which reaches a broader audience. However, even if attendance costs are not prohibitively expensive, the selection of abstracts may be highly competitive. As a result, not all research findings—even of topical interest—are selected. Furthermore, even if selection is conducted by independent experts, the limited information contained in an abstract may mask scientific and/or ethical shortcomings in the work.
Communication via abstracts is laudable, but should be rapidly followed by peer-reviewed publications, which allows for the findings to be comprehensively reviewed by experts. When abstracts remain the sole source of information, the findings’ significance might be misunderstood, overestimated or wrongly used to guide behaviours, policies and practices.
Preprints, that is, preliminary reports of work not yet peer-reviewed, are uploaded in dedicated free-access servers, such as https://www.medrxiv.org/ . Preprints are increasingly being used by health researchers, thanks to the evolving policies of major journals that now accept manuscripts previously posted as preprints. 17 Theoretically, preprints possess high value as they allow for rapid, open-access dissemination, and immediate yet informal peer-appraisal in the comments section. However, preprints also hold implicit risks. For instance, rapidity may detract from quality and accuracy; most peers will not be able to systematically invest time for the expected high-quality feedback; rushed or inexperienced readers may miss the (sometimes, small print) cautioning that preprints should not be considered established information, nor become the basis for informing policy or medical guidelines; and findings from preprints that may later be substantially revised or rejected after undergoing peer-review processes, could continue to be relied on and disseminated if, for example, they were included in scoping or systematic reviews before peer-review (the same applies to retracted peer-reviewed manuscripts).
To mitigate such risks, researchers should submit preprint manuscripts to a peer-reviewed journal as soon as reasonably possible, and transparently communicate on negative peer-review outcomes, or justify why the preprint is not being timeously submitted to a peer-review journal. Once accepted or published, researchers could remove their preprint from preprint servers or link to the final published version. The media have a duty to communicate preprint findings as unreviewed and subject to change. The scientific community should reach agreement on ‘Good Preprint Practices’ and ascribe less ambiguous terminology to preprints (eg, ‘Not peer-reviewed’ or ‘Peer-review pending’). 18
Press releases, media coverage and social media
Since 2021, the dissemination of clinical trial findings by corporate press release has almost become synonymous with announcements of COVID-19 scientific breakthroughs. Therefore, it seems important to briefly contextualise the strategy underpinning such dissemination. Corporate press releases are often preceded by stock repurchasing or ‘buybacks’, that is, companies buy back part of their own stock held by executives. This increases demand for the stock and enhances earnings per share. 19 Pharmaceutical or biotechnology companies typically engage in strategically timed buybacks, before press releases announcing significant research findings. Furthermore, corporates in the USA and elsewhere may employ press releases to comply with the legal requirements to disclose information that impact on their market values, and changes in their ‘financial conditions and operations’. 20 Press releases are typically drafted by marketing experts and they are often first aimed at the market, and driven by corporate interests rather than social value.
For researchers, the potential to amplify scientific visibility through mass media may act as a powerful incentive to indulge in flattering but inaccurate language. Nonetheless, they have a moral responsibility to review press releases for accuracy, and to immediately make key-information including the protocol, analysis plan and detailed results, publicly available. For instance, the media briefing that announced on 16 June 2020 the life-saving benefit of dexamethasone in severe COVID-19 was followed on 26 June by a preprint with full trial results 15 . In ab sence of such good practices, press releases can contain inaccuracies or overhype findings 7 with major damaging downstream effects. 16
The media have an equally significant impact on science dissemination: peer-reviewed publications which receive more attention from lay-press, are more likely to be cited in scientific literature. 21 Perceived media credibility also impacts on dissemination: once individuals trust a media source, 22 they often let down their guard on evaluating the credibility of that source. This speaks to the importance of discerning media dissemination ( box 2 ). Journalists who cover early press releases should critically appraise them considering their limitations and potential conflicts of interest.
Recommendations for journalists
Recommendations for journalists who cover (early) press release.
A. Always be conscious of the power of the media to shape the views, fears and beliefs of the public, in the short term, medium term and long term.
B. Weigh the tone and the extent of coverage afforded to press releases, based, among other factors, on:
A critical appraisal of whether the press release was preceded by stock buyouts and/or aimed at influencing corporates share values.
A critical appraisal of the science underpinning the press release, such as the sample size, study population representativeness (for instance, age, sex, ethnicity), research questions that are not addressed yet, and any omissions of potential harms.
A recourse to the views of independent scientists, paying attention to any declared or undeclared conflicts of interest that may bias their opinions.
C. Critically appraise the accuracy and possible biases of (independent) scientists’ opinions on press releases, when shared on personal social media feeds, before deciding whether to afford coverage to such views.
D. Afford the same coverage given to the initial press release (or more, if necessary) to any significant follow-up information-related thereto.
A call for good dissemination practices
The scientific community, health system policy-makers and regulators are the primary audience of peer-reviewed manuscripts, abstracts and preprints. These constituents should be, or become, ‘sufficiently skilled in critical thinking and scientific methods that they can make sensible decisions, regardless of whether an article is peer reviewed or not’ 15 ; understand that the nature of scientific knowledge is incremental and cumulative (one study seldom changes practice on its own); and also critically assess other sources, for example, pharmacovigilance, etc. Conversely, corporate press releases are aimed at influencing the market, and society as a whole—and not suited for scientific appraisal.
Irrespective of dissemination modalities, upstream information is cascaded to mainstream and social media, spreading knowledge but risk catalysing misunderstanding or overemphasis. Risks are only partially mitigated by independent quality control on the upstream information (relatively stringent in peer-review, weaker in preprints and abstracts, and virtually absent for press releases). In table 1 , we summarise recommendations for good dissemination practices, aimed at researchers, research institutions, developers, medical journals editors, media, journalists, social media actors, medical opinion leaders, policy-makers, regulators and the scientific community. All these stakeholders should integrate ethics and integrity in their policies and behaviours, to ensure timely, comprehensive, accurate, unbiased, unambiguous and transparent dissemination of research findings.
- View inline
Summary of the recommendations for good dissemination practices
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- The Unites States Agency for Healthcare Research and Quality
- National Institute for Health Care and Research
- World Medical Association
- Council for International Organizations of Medical Sciences (CIOMS)
- ↵ WHO guidelines on ethical issues in public health surveillance. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO. Accessed on 21/04/2022 at P214263_WHO Guidelines on Ethical Issues_COUV.indd .
- Massey DS ,
- Wallach JD , et al
- McMahon JH ,
- Lydeamore MJ ,
- Stewardson AJ
- Cashin AG ,
- Richards GC ,
- DeVito NJ , et al
- Upshur REG ,
- Zdravkovic M ,
- Berger-Estilita J ,
- Zdravkovic B , et al
- Ellingson MK ,
- Skydel JJ , et al
- Kmietowicz Z
- Ravinetto R
- Ravinetto R ,
- Caillet C ,
- Zaman MH , et al
- ↵ et al Sorkin AR , Karaian J , Gandel S . Biden Renews Pushback against stock Buybacks , 2022 . Available: https://www.nytimes.com/2022/03/28/business/dealbook/biden-stock-buybacks.html
- Neuhierl A ,
- Scherbina A ,
- Schlusche B
- Anderson PS ,
- Gray HM , et al
- Pew Research Centre
Twitter @RRavinetto
Contributors This manuscript was jointly written by RR and JAS.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Commissioned; externally peer reviewed.
Read the full text or download the PDF:
How to disseminate your research
- Published: 01 January 2019
- Version: V Version 1.0 - January 2019
This guide is for researchers who are applying for funding or have research in progress. It is designed to help you to plan your dissemination and give your research every chance of being utilised.
What does NIHR mean by dissemination?
Effective dissemination is simply about getting the findings of your research to the people who can make use of them, to maximise the benefit of the research without delay.
“Research is of no use unless it gets to the people who need to use it”
Professor Chris Whitty, Chief Scientific Adviser for the Department of Health
Principles of good dissemination
Stakeholder engagement: Work out who your primary audience is; engage with them early and keep in touch throughout the project, ideally involving them from the planning of the study to the dissemination of findings. This should create ‘pull’ for your research i.e. a waiting audience for your outputs. You may also have secondary audiences and others who emerge during the study, to consider and engage.
Format: Produce targeted outputs that are in an appropriate format for the user. Consider a range of tailored outputs for decision makers, patients, researchers, clinicians, and the public at national, regional, and/or local levels as appropriate. Use plain English which is accessible to all audiences.
Utilise opportunities: Build partnerships with established networks; use existing conferences and events to exchange knowledge and raise awareness of your work.
Context: Understand the service context of your research, and get influential opinion leaders on board to act as champions. Timing: Dissemination should not be limited to the end of a study. Consider whether any findings can be shared earlier
Remember to contact your funding programme for guidance on reporting outputs .
Your dissemination plan: things to consider
What do you want to achieve, for example, raise awareness and understanding, or change practice? How will you know if you are successful and made an impact? Be realistic and pragmatic.
Identify your audience(s) so that you know who you will need to influence to maximise the uptake of your research e.g. commissioners, patients, clinicians and charities. Think who might benefit from using your findings. Understand how and where your audience looks for/receives information. Gain an insight into what motivates your audience and the barriers they may face.
Remember to feedback study findings to participants, such as patients and clinicians; they may wish to also participate in the dissemination of the research and can provide a powerful voice.
When will dissemination activity occur? Identify and plan critical time points, consider external influences, and utilise existing opportunities, such as upcoming conferences. Build momentum throughout the entire project life-cycle; for example, consider timings for sharing findings.
Think about the expertise you have in your team and whether you need additional help with dissemination. Consider whether your dissemination plan would benefit from liaising with others, for example, NIHR Communications team, your institution’s press office, PPI members. What funds will you need to deliver your planned dissemination activity? Include this in your application (or talk to your funding programme).
Partners / Influencers: think about who you will engage with to amplify your message. Involve stakeholders in research planning from an early stage to ensure that the evidence produced is grounded, relevant, accessible and useful.
Messaging: consider the main message of your research findings. How can you frame this so it will resonate with your target audience? Use the right language and focus on the possible impact of your research on their practice or daily life.
Channels: use the most effective ways to communicate your message to your target audience(s) e.g. social media, websites, conferences, traditional media, journals. Identify and connect with influencers in your audience who can champion your findings.
Coverage and frequency: how many people are you trying to reach? How often do you want to communicate with them to achieve the required impact?
Potential risks and sensitivities: be aware of the relevant current cultural and political climate. Consider how your dissemination might be perceived by different groups.
Think about what the risks are to your dissemination plan e.g. intellectual property issues. Contact your funding programme for advice.
More advice on dissemination
We want to ensure that the research we fund has the maximum benefit for patients, the public and the NHS. Generating meaningful research impact requires engaging with the right people from the very beginning of planning your research idea.
More advice from the NIHR on knowledge mobilisation and dissemination .

- Request new password
- Create a new account
Doing Research in Counselling and Psychotherapy
Student resources, disseminating the findings of your research study.
It is very important to find appropriate ways to disseminate the findings of your research – projects that sit on office or library shelves and are seldom or never read represent a tragic loss to the profession.
A key dimension of research dissemination is to be actively involved with potential audiences for your work, and help them to understand what it means to them. These dialogues also represent invaluable learning experiences for researchers, in terms of developing new ideas and appreciating the methodological limitations of their work. An inspiring example of how to do this can be found in:
Granek, L., & Nakash, O. (2016). The impact of qualitative research on the “real world” knowledge translation as education, policy, clinical training, and clinical practice. Journal of Humanistic Psychology , 56(4), 414 – 435.
A further key dimension of research dissemination lies in the act of writing. There are a number of challenges associated with writing counselling and psychotherapy research papers, such as the need to adhere to journal formats, and the need (sometimes) to weave personal reflective writing into a predominantly third-person standard academic style. The items in the following sections explore these challenges from a variety of perspectives.
Suggestions for becoming a more effective academic writer
Sources of advice on how to ease the pain of writing:
Gioia, D. (2019). Gioia’s rules of the game. Journal of Management Inquiry , 28(1), 113 – 115.
Greenhalgh, T. (2019). Twitter women’s tips on academic writing: a female response to Gioia’s rules of the game. Journal of Management Inquiry , 28(4), 484 – 487.
Roulston, K. (2019). Learning how to write successfully from academic writers. The Qualitative Report, 24(7), 1778 – 1781.
Writing tips from the student centre, University of Berkeley
The transition from being a therapist to being a researcher
Finlay, L. (2020). How to write a journal article: Top tips for the novice writer. European Journal for Qualitative Research in Psychotherapy , 10, 28 – 40.
McBeath, A., Bager-Charleson, S., & Abarbanel, A. (2019). Therapists and academic writing: “Once upon a time psychotherapy practitioners and researchers were the same people”. European Journal for Qualitative Research in Psychotherapy , 9, 103 – 116.
McPherson, A. (2020). Dissertation to published article: A journey from shame to sharing. European Journal for Qualitative Research in Psychotherapy , 10, 41 – 52.
Journal article style requirements of the American Psychological Association (including a section on writing quantitative papers)
Writing qualitative reports
Jonsen, K., Fendt, J., & Point, S. (2018). Convincing qualitative research: What constitutes persuasive writing? Organizational Research Methods , 21(1), 30 – 67.
Ponterotto, J.G. & Grieger, I. (2007). Effectively communicating qualitative research. The Counseling Psychologist , 35, 404 – 430.
Smith, L., Rosenzweig, L. & Schmidt, M. (2010). Best practices in the reporting of participatory action research: embracing both the forest and the trees. The Counseling Psychologist, 38, 1115 – 1138.
Staller, K.M. & Krumer-Nevo, M. (2013). Successful qualitative articles: A tentative list of cautionary advice. Qualitative Social Work, 12, 247 – 253.
Clark, A.M. & Thompson, D.R. (2016). Five tips for writing qualitative research in high-impact journals: moving from #BMJnoQual . International Journal of Qualitative Methods , 15, 1 – 3
Gustafson, D. L., Parsons, J. E., & Gillingham, B. (2019). Writing to transgress: Knowledge production in feminist participatory action research. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research, 20 . DOI: 10.17169/fqs-20.2.3164
Caulley, D.N. (2008). Making qualitative reports less boring: the techniques of writing creative nonfiction. Qualitative Inquiry, 14, 424 – 449.
Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks
Affiliation.
- 1 Centre for Reviews and Dissemination, University of York, YO10 5DD, UK. [email protected].
- PMID: 21092164
- PMCID: PMC2994786
- DOI: 10.1186/1748-5908-5-91
Background: Addressing deficiencies in the dissemination and transfer of research-based knowledge into routine clinical practice is high on the policy agenda both in the UK and internationally.However, there is lack of clarity between funding agencies as to what represents dissemination. Moreover, the expectations and guidance provided to researchers vary from one agency to another. Against this background, we performed a systematic scoping to identify and describe any conceptual/organising frameworks that could be used by researchers to guide their dissemination activity.
Methods: We searched twelve electronic databases (including MEDLINE, EMBASE, CINAHL, and PsycINFO), the reference lists of included studies and of individual funding agency websites to identify potential studies for inclusion. To be included, papers had to present an explicit framework or plan either designed for use by researchers or that could be used to guide dissemination activity. Papers which mentioned dissemination (but did not provide any detail) in the context of a wider knowledge translation framework, were excluded. References were screened independently by at least two reviewers; disagreements were resolved by discussion. For each included paper, the source, the date of publication, a description of the main elements of the framework, and whether there was any implicit/explicit reference to theory were extracted. A narrative synthesis was undertaken.
Results: Thirty-three frameworks met our inclusion criteria, 20 of which were designed to be used by researchers to guide their dissemination activities. Twenty-eight included frameworks were underpinned at least in part by one or more of three different theoretical approaches, namely persuasive communication, diffusion of innovations theory, and social marketing.
Conclusions: There are currently a number of theoretically-informed frameworks available to researchers that can be used to help guide their dissemination planning and activity. Given the current emphasis on enhancing the uptake of knowledge about the effects of interventions into routine practice, funders could consider encouraging researchers to adopt a theoretically-informed approach to their research dissemination.
Grants and funding
- MC_U130085862/MRC_/Medical Research Council/United Kingdom
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Ten tips to improve the visibility and dissemination of research for policy makers and practitioners
J p tripathy, a bhatnagar, h d shewade, a m v kumar, r zachariah, a d harries.
- Author information
- Article notes
- Copyright and License information
CORRESPONDENCE Jaya Prasad Tripathy, International Union Against Tuberculosis and Lung Disease South-East Asia Office, C-6 Qutub Institutional Area, New Delhi, 110 016 India, e-mail: [email protected] , [email protected]
Corresponding author.
Received 2016 Oct 7; Accepted 2017 Dec 2; Issue date 2017 Mar 21.
Effective dissemination of evidence is important in bridging the gap between research and policy. In this paper, we list 10 approaches for improving the visibility of research findings, which in turn will hopefully contribute towards changes in policy. Current approaches include using social media (Facebook, Twitter, LinkedIn); sharing podcasts and other research outputs such as conference papers, posters, presentations, reports, protocols, preprint copy and research data (figshare, Zenodo, Slideshare, Scribd); and using personal blogs and unique author identifiers (ORCID, ResearcherID). Researchers and funders could consider drawing up a systematic plan for dissemination of research during the stage of protocol development.
Keywords: open access, Twitter, Facebook, social media, policy brief
Une dissémination efficace des résultats de recherche est cruciale pour combler le fossé qui existe entre la recherche et la politique de santé, ainsi que sa mise en œuvre. Dans cet article, nous énumérons 10 approches visant à améliorer la visibilité des résultats de la recherche qui vont, si tout va bien, à leur tour contribuer au changement en matière de politique. Les approches actuelles incluent le recours aux réseaux sociaux (Facebook, Twitter, LinkedIn), le partage de podcasts et d'autres résultats de recherche comme des documents de conférences, des affiches, des présentations, des rapports, des protocoles, des photocopies, des données de recherche (figshare, Zenodo, Slideshare, Scribd), l'utilisation d'un blog personnel et un identifiant unique de l'auteur (ORCID, ResearcherID). Les chercheurs et les financeurs pourraient envisager d'ébaucher un plan systématique de dissémination de la recherche dès l'élaboration du protocole.
Es importante lograr una difusión eficaz de las pruebas científicas, con el objeto de superar la brecha que existe entre la investigación y las políticas y las prácticas. En el presente artículo se mencionan diez enfoques que mejoran la visibilidad de los resultados de las investigaciones, con la intención de que contribuyan a su vez a la modificación de las políticas. Las estrategias vigentes incluyen la utilización de las redes sociales (Facebook, Twitter, LinkedIn), el intercambio de las redifusiones multimedia (podcasts) y de otros productos de las investigaciones como son los artículos, los afiches, las presentaciones en las conferencias, los informes, los protocolos, los manuscritos antes de su publicación, los datos de investigación (figshare, Zenodo, Slideshare, Scribd) y la utilización de bitácoras personales (blogs) y de los identificadores únicos de los investigadores (ORCID, ResearcherID). Los investigadores y las instituciones patrocinadoras deben procurar la elaboración de un plan sistemático de difusión de las investigaciones durante la etapa de preparación del protocolo.
The full potential for research evidence to influence changes in decision-making and policy and practice is not yet being realised. 1 Keeping in mind the growing interest in bridging the gap between research and policy and practice, effective dissemination in an appropriate format is of vital importance. If we wish to maximise the benefits of publication and its eventual influence on policy and practice, there are a number of actions that can be taken before and after the paper is published.
As Danny Iny wrote in his blog, ‘Sure, content is king—but without an audience, the king can get awfully lonely’. 2 Even when the content is great it does not find an audience on its own. There is thus a need for a strategy to find and attract an audience.
According to the World Health Organization (WHO), a number of dissemination tools are available to researchers, including research reports, peer-reviewed publications, press releases and policy briefs. 3 In today's world of information overload, the scholarly community is also turning its attention to the use of social media and other online platforms. Not surprisingly, in recent years academics have shown a growing interest in non-traditional methods of evaluating their scholarly ‘impact’. These alternative metrics, known as ‘altmetrics’, allow researchers to gauge the impact and reach of their research in the social web beyond the traditional science citation count and journal impact factors.
In this paper, we enlist 10 ‘can't miss’ approaches to improve the visibility of research findings, which will in turn hopefully contribute towards changes in policy and/or practice, although we acknowledge the fact that application of research findings in making decisions about health care is complex. Effective dissemination, however, is certainly the way to get people talking about it ( Table ).
Ten tips to improve the visibility and dissemination of research findings
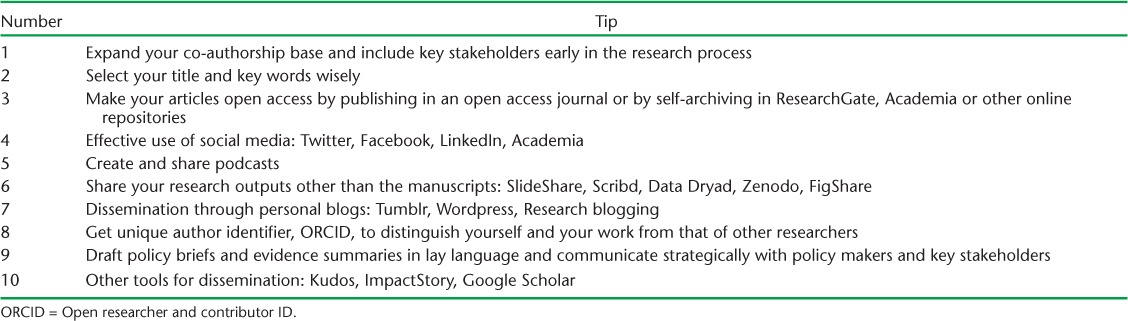
10 TIPS FOR IMPROVING RESEARCH VISIBILITY
Expand your co-authorship base.
In addition to the usual benefit of bringing new expertise and ideas to the paper, co-authoring with a diverse group of colleagues helps to disseminate research findings more widely. 4 , 5 To impact changes in policy and/or practice, potential policy makers should be engaged early on, preferably right from the conception of the research question, through the conduct of the study and to eventual publication. The approach of involving policy makers early on in the process fosters a sense of ownership and responsibility, which is key to bringing about any change in policy and/or practice. 6 , 7
Select your title and keywords wisely
Title and keywords have the potential to significantly impact the chances of getting picked up when searched, read, cited and included in systematic reviews that synthesise evidence on an issue. 8
Journals, search engines, and indexing and abstracting services classify papers using keywords. An accurate list of keywords will therefore ensure correct indexing and help showcase the research to attract interested groups. It is best to select keywords from a list of key terms/phrases that are used repeatedly in the text and preferably not repeated in the title or abstract. It is recommended to use the Medical Subject Headings (MeSH) tool to choose keywords. MeSH is a comprehensive, controlled vocabulary for the purpose of indexing journal articles and books for the MEDLINE database (US National Library of Medicine ® , Bethesda, MD, USA). The title should be simple, clear and catchy, while describing the study appropriately. It is strategic to think about terms that readers might use to search for the study and include them in the title. Abbreviations and jargon are best avoided.
Make your articles open access
Open access articles have the advantage of being accessible to all readers free of charge, including policy makers, which increases the chance of being cited by the readers. 9–11 Publishing in an open access journal will make the paper available to all readers free of charge.
Self-archiving is the act of the author depositing a free copy of an electronic document online in order to provide immediate open access to it. ResearchGate (Berlin, Germany) and Academia.edu (San Francisco, CA, USA) are free online repositories where published work can be shared for wider circulation and greater visibility of research and where there can be better connection and interaction with peers. Authors can also put their articles in institutional repositories, but prior to doing so it is important to check on the self-archiving policy of the publisher. For example, the Médecins Sans Frontières (MSF, Geneva, Switzerland) repository ( http://fieldresearch.msf.org/msf/ ) hosts full free-text articles on field research conducted in several countries published in over 100 peer-reviewed journals.
Effective use of online social media
Many studies have shown that there is a statistically significant correlation between social media mentions such as posts, tweets, blogs and citation counts. 12 , 13
Authors need to engage with individuals and groups within and beyond academia, including key policy influencers and decision makers, and with individuals with shared interests through Facebook posts (Facebook Inc, San Francisco, CA, USA) and tweets, joining Linked In (LinkedIn Corp, Mountain View, CA, USA), Academia.edu and other groups, sharing research and commenting on blogs. There needs to be proactive engagement with researchers, non-governmental organisations, patient groups or other groups that might be interested in the work, and to engage them through various online social platforms. Policy makers or key decision makers/influencers also need to be engaged through various social media channels to keep them informed of the research evidence generated ( Figure ).

Improving visibility and dissemination of research.
Authors can create an account on Twitter (Twitter Inc, San Francisco, CA, USA) ( https://twitter.com/ ) and add a short description of 160 characters or less stating their experience, research interests, organisational affiliation and a link to personal blogs, if any. They can engage with other researchers, policy makers and the public by finding users who share common interests and electing to ‘follow’ them to start receiving their updates. Twitter makes it easy to find other people to follow via their ‘Who to follow’ panel.
Authors can tweet on a variety of subjects: research publications and findings, opinions on a study, news or blogposts relevant to their topics of interest, recent developments in their field. Tagging sector specialist journalists will help in promoting and increasing the searchability of the research paper. Tagging policy makers will bring an author's piece of evidence into the limelight within policy circles.
The hashtag (#) is the most widely used means of classifying content on social media. It makes one's own content searchable and allows one to find relevant content from related areas. The hashtag also allows one to connect with and engage other social media users based on a common theme or interest. The more focused and exact the hashtag, the more targeted the audience will be—and a targeted audience generally means better engagement. Making infographic summaries of research findings helps in gaining attention and rapid dissemination using social media, as images are easier to share.
Every social media platform offers the facility to form thematic groups or clubs. Adding relevant people to a like-minded, subject-related group will create a personalised channel to reach a larger number of target audiences and ensure reception. Do share your social media coordinates for people who want to connect with you.
MethodSpace ( www.methodspace.com ) (Sage Publications, Thousand Oaks, CA, USA), OR network ( http://ornetwork.ning.com/ ) and the Social Science Research Network (SSRN, Rochester, NY, USA) ( http://ssrn.com/en/ ) are social network services for social and medical scientists where one can ask questions on forums, discuss research, connect to other researchers in the field and blog about one's own latest research.
LinkedIn ( www.linkedin.com ) is a professional networking site for professionals in which people can create a profile, connect with peers and network. Authors can list their publications and other research outputs, experiences, skills and current and past positions.
Academia.edu is another multidisciplinary academic networking site. It has a strong profile and curriculum vitae feature and is excellent for showcasing achievements, publications and expertise. Available measures of impact include counts for profile views, document views, document downloads, unique visitors, external links to documents, geographic distribution of visitors and referrals.
Create and share podcasts
Creating a podcast (an audio or video file in digital format for automatic download over the Internet) describing the research project and key findings and posting it to YouTube (YouTube LLC, San Bruno, CA, USA) or Vimeo (InterActive Corp, New York, NY, USA), or sharing them in social media platforms such as Twitter, Facebook or your personal blog, will help in rapid dissemination.
Sharing research outputs other than the manuscript
In addition to published articles, preprints, conference papers and posters, presentations, reports, working papers, protocols, preprint copy, research data and videos are all evidence of your research activity. By making them all publicly accessible you can increase visibility, preserve your output and make it available for future use.
Slideshare (LinkedIn Corp, Mountain View, CA, USA) and Scribd (Scribd Inc, San Francisco, CA, USA), while not exclusive to the research community, are useful for sharing presentations and keynotes and providing basic usage statistics. F1000 Research (Science Navigation Group, London, UK) is an option for researchers in the life sciences that allows free deposit of research posters and presentations. Publishing research data in Data Dryad (Dryan, Durham, NC, USA) or via multi-purpose services such as figshare (London, UK) ( http://figshare.com/ ) or Zenodo (Geneva, Switzerland) ( https://zenodo.org/ ) for a range of outputs will improve visibility.
Create a personal blog
Create a personal blog where you can share your thoughts, research ideas and/or key findings, promote your work, or write case studies of how your work has impacted others. Blogging platforms such as wordpress.com (Automattic Inc, San Francisco, CA, USA) or tumblr.com (Tumblr Inc, New York, NY, USA) are quick and easy tools for creating a blog.

Get a unique author identifier ORCID to distinguish yourself and your work from other researchers.
Using a consistent name throughout a research career facilitates easy retrieval of a researcher's output. Common problems with a consistent author name include inconsistent name formats, legal name changes, highly similar names or common names, which can make it difficult to associate research output to the correct author.
It has been suggested that using an author identification system such as ORCID (Open Researcher and Contributor ID) (ORCID Inc, Bethesda, MD, USA) or ResearcherID (Thomson Reuters Corp, New York, NY, USA) could help. ORCID IDs are permanent identifiers for researchers. They protect your unique scholarly identity and help you keep your publication record updated with very little effort. After you have created an ORCID account, you can link it to your Google Scholar (Google Inc, Mountain View, CA, USA) and LinkedIn profiles, your personal website and any other websites where you have a scholarly profile.
Lay language policy briefs/evidence summaries for policy makers
A lay language policy brief is a short, to the point, jargon-free document written for non-specialists, especially policy makers or those who can influence policy. It presents research findings/evidence to policy actors and other key stakeholders, highlighting the relevance of the specific research to policy and offering recommendations for change. This is an effective way of bringing important research to the attention of policy actors as they can be read in a short amount of time.
Other tools for dissemination
Present your study findings at conferences or any academic gatherings. Include your Twitter handle and links to some of your profiles in presentations, an e-mail signature and business card. Researchers can use their institutional newsletter/bulletin/local newspaper to disseminate study findings in layman language.
Kudos (Oxford, UK) ( https://www.growkudos.com/ ) and ImpactStory ( https://impactstory.org/ ) are powerful tools that help researchers promote their research outputs together with measures of their impact. They allow authors to showcase their publications by creating links to full texts and including additional information such as a short title, a lay language explanation, an impact statement and links to additional related content, such as underlying data, code, video, slides, or other elements. In addition, it offers a streamlined process for sharing your content via social media and allows you to monitor the results of that activity through the number of tweets, posts, visits, downloads and views, and a score generated by Altmetric.com .
Google Scholar is by far the most widely used bibliographical tool for scholarly publications. Create an account in Google Scholar and go to ‘My citation’. The profile shows your list of publications in Google Scholar, with basic metrics. You can use the citation alert in Google Scholar to notify you whenever your article is cited in the scholarly web. A benefit of Google Scholar Profiles is that they function as a landing page for your name and your publications, although this functionality only works if your profile is set to Public. Thus it increases the ‘Google-ability’ of your profile.
To highlight a real project experience, in the European project SOPHIE (Evaluating the Impact of Structural Policies on Health Inequalities and Their Social Determinants and Fostering Change), dissemination was one of the key objectives to achieve the purpose of fostering policy change based on research findings. The use of online platforms (website, Twitter, and Slideshare), production of informative videos, partnership with civil society organisations and organisation of final concluding scientific events enabled wider dissemination within the scientific community, civil society, and policy circles, and influenced public view on the impact on health and equity of certain policies. 14 Similarly, the Agency for Healthcare Research Quality, through their Translating Research into Practice (TRIP) initiative, has shown commitment in disseminating research results through a dissemination framework involving multiple methods and tools which has led to improved patient care practices, thus ultimately making the health care system safer. 15
Considering the key role of dissemination in knowledge translation continuum, funders should demand some commitment or effort on the part of grant holders to disseminate the findings of their research. The Economic and Social Research Council, UK, has made a dissemination framework available to grant applicants or holders. 16 A plan of dissemination including a social media strategy or any of the dissemination products such as a project video, monograph, newsletter, bulletin, press release, policy brief, poster, infographic summary, dissemination workshop or project website, etc., could be budgeted in the grant proposal.
Given the current emphasis on enhancing the uptake of evidence into routine practice and policy making, both researchers and funders could consider drawing up a systematic plan for research dissemination during the stage of proposal development. Re searchers should learn the art of using social media and other on line platforms to increase the dissemination of their work. Involvement of policy influencers and decision makers right from the beginning of the conception of the research question is the most crucial step in enhancing policy uptake.
Acknowledgments
The authors are grateful to A Ramsay, Special Programme for Research and Training in Tropical Diseases, World Health Organization, Geneva, Switzerland, for his valuable comments while preparing the manuscript. The authors thank the Department for International Development, London, UK, for funding the Global Operational Research Fellowship Programme in which JPT works as an operational research fellow. La Fondation Veuve Emile Metz-Tesch (Luxembourg) supported the open access publication costs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest: none declared.
- 1. Wilson P M, Petticrew M, Calnan M W, Nazareth I.. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci 2010; 5: 91. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Iny D. Four proven strategies for finding a wider audience for your content. Boulder, CO, USA: Rainmaker Digital, 2012. http://www.copyblogger.com/targeted-content-marketing/ Accessed January 2017. [ Google Scholar ]
- 3. World Health Organization. . Disseminating the research findings. Geneva, Switzerland: WHO, 2014. http://www.who.int/tdr/publications/year/2014/participant-workbook5_030414.pdf Accessed January 2017. [ Google Scholar ]
- 4. Aksnes D W. Characteristics of highly cited papers. Res Eval 2003; 1 2: 159– 170. [ Google Scholar ]
- 5. Wuchty S, Jones B F, Uzzi B.. The increasing dominance of teams in production of knowledge. Science 2007; 316: 1036– 1039. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Kumar A M V, Satyanarayana S, Wilson N C, . et al. Operational research leading to rapid national policy change: tuberculosis-diabetes collaboration in India. Public Health Action 2014; 4: 85– 88. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Walley J, Khan M A, Shah S K, Witter S, Wei X.. How to get research into practice: first get practice into research. Bull World Health Organ 2007; 85: 424. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Ebrahim N A, Salehi H, Embi M A, . et al. Effective strategies for increasing citation frequency. International Education Studies 2013; 6: 93– 99. [ Google Scholar ]
- 9. Lawrence S. Free online availability substantially increases a paper's impact Nature 2001; 411: 21. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Gargouri Y, Hajjem C, Larivière V, . et al. Self-selected or mandated, open access increases citation impact for higher quality research. PLOS ONE 2010; 5: e13636. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Zachariah R, Rust S, Berger S D, . et al. Building global capacity for conducting operational research using the SORT IT model: where and who? PLOS ONE 2016; 11: e0160837. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Eysenbach G. Can tweets predict citations? Metrics of social impact based on Twitter and correlation with traditional metrics of scientific impact. Med Internet Res 2011; 13: e123. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Thelwall M, Haustein S, Larivière V, Sugimoto C R.. Do altmetrics work? Twitter and ten other social web services. PLOS ONE 2013; 8: e64841. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Marin-Gonzalez E, Malmusi D, Camprubi L, Borrell C.. The role of dissemination as a fundamental part of a research project: lessons learned from SOPHIE. Int J Health Serv 2016; Epub ahead of print. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Carpenter D, Nieva V, Albaghal T, . et al. Development of a planning tool to guide research dissemination. : Henriksen K, Battles J B, Marks E S, et al. Advances in patient safety: from research to implementation. Rockville, MD, USA: Agency for Healthcare Research and Quality, 2005. [ PubMed ] [ Google Scholar ]
- 16. Economic and Social Research Council. . Communications strategy: a step-by-step guide. Swindon, UK: Economic and Social Research Council, 2004. [ Google Scholar ]
- View on publisher site
- PDF (210.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Part 1. Overview Information
National Institutes of Health ( NIH )
National Human Genome Research Institute ( NHGRI )
National Institute on Aging ( NIA )
National Institute on Alcohol Abuse and Alcoholism ( NIAAA )
Eunice Kennedy Shriver National Institute of Child Health and Human Development ( NICHD )
National Institute of Dental and Craniofacial Research ( NIDCR )
National Institute on Drug Abuse ( NIDA )
National Institute of Environmental Health Sciences ( NIEHS )
National Institute of Mental Health ( NIMH )
National Institute of Neurological Disorders and Stroke ( NINDS )
Fogarty International Center ( FIC )
Tribal Health Research Office ( THRO )
All applications to this funding opportunity announcement should fall within the mission of the Institutes/Centers. The following NIH Offices may co-fund applications assigned to those Institutes/Centers.
Division of Program Coordination, Planning and Strategic Initiatives, Office of Disease Prevention ( ODP )
Office of Behavioral and Social Sciences Research ( OBSSR )
R03 Small Grant Program
- April 4, 2024 - Overview of Grant Application and Review Changes for Due Dates on or after January 25, 2025. See Notice NOT-OD-24-084 .
- August 31, 2022 - Implementation Changes for Genomic Data Sharing Plans Included with Applications Due on or after January 25, 2023. See Notice NOT-OD-22-198 .
- August 5, 2022 - Implementation Details for the NIH Data Management and Sharing Policy. See Notice NOT-OD-22-189 .
PAR-25-144 , R01 Small Research Grants PAR-25-143 , R21 Exploratory/Developmental Grants
See Section III. 3. Additional Information on Eligibility .
The purpose of this Notice of Funding Opportunity (NOFO) is to support studies that will identify, develop, and/or test strategies for overcoming barriers to the adoption, adaptation, integration, sustainability, scale-up, and spread of evidence-based interventions, practices, programs, tools, treatments, guidelines, and policies (herein referred to collectively as evidence-based interventions). Studies that promote equitable dissemination and implementation of evidence-based interventions among underrepresented communities are encouraged. Conversely, there is a benefit in understanding circumstances that create a need to stop or reduce (de-implement) the use of practices that are ineffective, unproven, low-value, or harmful. In addition, studies to advance dissemination and implementation research methods and measures are encouraged. Applications that focus on re-implementation of evidence-based health services that may be disrupted amidst disasters (e.g., pandemics, climate change) remain relevant.
All applications must be within the scope of the mission of one of the Institutes/Centers listed above.
This Notice of Funding Opportunity (NOFO) requires a Plan for Enhancing Diverse Perspectives (PEDP).
30 days prior to the application due date
All applications are due by 5:00 PM local time of applicant organization.
Applicants are encouraged to apply early to allow adequate time to make any corrections to errors found in the application during the submission process by the due date.
Not Applicable
It is critical that applicants follow the instructions in the Research (R) Instructions in the How to Apply - Application Guide , except where instructed to do otherwise (in this NOFO or in a Notice from NIH Guide for Grants and Contracts ).
Conformance to all requirements (both in the Application Guide and the NOFO) is required and strictly enforced. Applicants must read and follow all application instructions in the Application Guide as well as any program-specific instructions noted in Section IV. When the program-specific instructions deviate from those in the Application Guide, follow the program-specific instructions.
Applications that do not comply with these instructions may be delayed or not accepted for review.
IMPORTANT: Per NOT-OD-24-086 updated application forms (FORMS-I) will be used for this opportunity. The updated forms are not yet available and will be posted 30 calendar days or more prior to the first application due date. Once posted, you will be able to access the forms using one of the following submission options:
- An institutional system-to-system (S2S) solution
- Grants.gov Workspace
Part 2. Full Text of Announcement
Section i. notice of funding opportunity description.
Each year, billions of U.S. tax dollars are spent on research and hundreds of billions are spent on delivery of health interventions, healthcare services, and public health programs in clinical and community settings. However, relatively little is spent on research to understand how best to ensure that the lessons learned from research are relevant to inform and improve the quality of health, delivery of services, and the utilization and sustainability of evidence-based interventions. For years, we have known of the limitations of research publications in leading to widespread uptake of evidence-based interventions, but too often the scientific pathway ends prematurely, before we can determine the best ways to improve equitable dissemination, adoption, implementation, sustainability, scale and spread. Given the interest and investment in intervention trials that seek to determine the optimal interventions to be used in clinical and community settings, it is essential that practitioners (e.g., healthcare providers, public health practitioners), consumers, families, caregivers, communities (e.g., workplace, school, place of worship), healthcare practice settings, and policymakers are equipped with empirically-supported strategies to integrate scientific knowledge and effective health interventions into everyday use. The National Institutes of Health has recognized that closing the gap between biomedical or basic behavioral discovery, population health, and healthcare delivery and public health is both a complex challenge and an absolute necessity if we are to ensure that all populations benefit from the Nation’s investments in scientific discoveries.
For many years, health researchers may have assumed that interventions would be readily adopted and implemented once their evidence was established; however, compelling and robust research suggests that this has not been the case. Even when interventions have been tested within effectiveness studies, the development of knowledge to support their broader dissemination and implementation (e.g., cost and financing of the intervention, practitioner training, availability of resources, integration into community or healthcare systems, delivery to underserved or under-resourced populations, monitoring the quality or equity of intervention delivery) has often remained outside the scope of these large-scale clinical trials. This has also been the case for the dissemination and implementation of policies and guidelines.
Dissemination and implementation research intends to bridge the gap between research, practice, and policy by building a knowledge base about how health information, effective interventions, and new clinical practices, guidelines, and policies are communicated and integrated for public health and health care service use in specific settings.
For the purpose of this NOFO, we make a distinction between "dissemination research" and "implementation research", as follows:
Dissemination research is defined as the scientific study of the targeted distribution of information and intervention materials to a specific public health, clinical practice, or policy audience. The intent is to understand how best to communicate and integrate knowledge and the associated evidence-based interventions.
We are currently missing critical information about how, when, by whom, and under what circumstances evidence spreads throughout communities, organizations, front line workers and consumers of public health and clinical services. As a prerequisite for unpacking how information can lead to intervention or service changes, we need to understand how and why information on physical and behavioral health, preventive services, disease management, decision making, and other effective interventions may or may not reach stakeholders. We need to understand what underlies the creation, transmission, and reception of information on evidence-based pharmacological, behavioral, psychosocial, genomic, policy, and systems interventions. Successful dissemination of evidence for effective health interventions may occur quite differently depending on whether the audience consists of consumers, caregivers, practitioners, policymakers, employers, administrators, or other stakeholder groups. Moving the field forward will require studies identifying mechanisms and communication approaches to package and convey the evidence necessary to improve public health, community, and healthcare services in ways relevant to local settings.
Implementation research is defined as the scientific study of the use of strategies to adopt and integrate evidence-based health interventions into clinical and community settings to improve individual outcomes and benefit population health.
Implementation research seeks to understand the behavior of practitioners and support staff, organizations, consumers and family members, and policymakers in context as key influences on the adoption, implementation, sustainability, scale and spread of evidence-based health interventions. Implementation studies should not assume that effective interventions can be integrated into any service setting and for consumer groups and populations without attention to local context, nor that a unidirectional flow of information (e.g., publishing a recommendation, trial, or guideline) is sufficient to achieve practice change. Relevant studies should develop a knowledge base about "how" evidence-based interventions are integrated within diverse practice settings and patient populations, which likely will require more than the distribution of information about the interventions. This research announcement encourages studies to test models, theories, and conceptual frameworks of the implementation process that move away from an exclusively "top-down" or reductionist approach to a greater emphasis on the resources of local care settings and the needs of multiple key interested parties, including approaches such as systems science, team science, community engaged research, participatory action research, citizen science, and related approaches that engage stakeholders and end-users throughout the research process.
Dissemination and Implementation (D&I) Research: Broadly, studies in this field typically involve multidisciplinary teams, interdisciplinary cooperation, and even transdisciplinary collaboration, utilizing theories, empirical findings, and methods from a variety of scientific disciplines. Relevant fields include but are not limited to: information science, organizational and management theory, health economics, behavioral science, public health, business and public administration, statistics, anthropology, psychology, epidemiology, decision science, engagement science, systems science, health equity research, engineering, and marketing. D&I research will often include significant and ongoing collaboration with stakeholders from multiple public health and/or clinical practice settings as well as consumers of services and their families/social networks. This NOFO will support a variety of rigorous study designs including (but not limited to) observational, experimental, quasi-experimental, and simulation modeling that produce evidence on relevant outcomes (e.g., acceptability, feasibility, adoption, fidelity, penetration, sustainability), costs, and/or unanticipated consequences of dissemination and implementation efforts. The goal is to conduct dissemination and implementation studies utilizing research designs and measures that are rigorous, relevant, and low burden when possible. Studies of dissemination or implementation strategies should attempt to build knowledge both on the overall effectiveness of the strategies, as well as "how and why" they work. Data on mechanisms of action, moderators and mediators, and costs of dissemination and implementation strategies will greatly aid decision-making on which strategies work for which interventions, in which settings, for what populations, and under what conditions.
For additional resources on dissemination and implementation research, including information on D&I training opportunities, funded studies, key references, past workshops and conferences, visit: http://cancercontrol.cancer.gov/is/ ; and https://prevention.nih.gov/research-priorities/dissemination-implementation .
Specific Objectives and Scope of this NOFO
This NOFO invites research grant applications to advance the science of dissemination and implementation in health that are consistent with the size and scope of objectives in the R03 small research grant funding mechanism. Studies that are larger in size, scope, and objectives are encouraged to apply to the R21 exploratory/development grant program or R01 research project grant program. Below are examples of types of studies and focus areas that are consistent with the objectives of this NOFO and generally reflect the size and scope of the budget and timeline of the R03 small research grant program that can be carried out in a short period of time with limited resources, that may set up subsequent studies.
Examples of relevant research topics include but are not limited to:
- Studies that use primary data collection (e.g., surveys) or secondary data (e.g., claims data) to identify factors that contribute to the long-term sustainment of evidence-based interventions in public health and clinical practice.
- Studies that conduct economic evaluations (e.g., budget impact analysis, return-on-investment analysis) of dissemination and implementation strategies.
- Studies of influences on the creation, packaging, transmission, and reception of information about evidence-based interventions to key partners and implementers.
- Studies that use secondary data (e.g., administrative data, claims data) to understand variations in the effectiveness of strategies for de-implementing clinical and community practices that are ineffective, unproven, low-value, or harmful.
- Studies on the development of novel methodological, statistical, systems modeling, and analytical approaches for a range of types of D&I studies.
- Studies that focus on empirical testing of theories, models, and frameworks for D&I determinants, processes, and outcomes using primary or secondary data and robust statistical modeling procedures.
- Studies that develop psychometrically sound and robust D&I-related measures and instruments, which includes (but is not limited to) testing for multiple types of validity (e.g., construct validity, predictive validity) and reliability (e.g., internal consistency, temporal stability) and assessing for practicality and utility.
- Studies that develop pragmatic and actionable measures to guide selection, continuation, and/or discontinuation of the use of particular implementation strategies over time.
- Studies to better understand the relationship between strength or level of evidence of an intervention and decision-making processes among key partners to adopt and implement (or de-adopt and de-implement) the intervention.
- Studies to develop and refine tools and techniques for advancing qualitative and ethnographic methods in D&I research (e.g., rapid qualitative analysis, cross-study qualitative data collection and analytical procedures, and efficient ethnographic data collection and analysis) to enhance contextual understanding of implementation.
- Studies to develop robust methods and measures to support rapid, data-driven, and equitable adaptation of implementation strategies across implementation phases and implementation contexts.
- Studies on effective and collaborative approaches and processes for sharing qualitative, quantitative, and/or mixed methods D&I-related data with researchers, practitioners, and clinical and community partners that is actionable and mutually beneficial.
- Studies on how to effectively and equitably engage researchers, practitioners, policymakers, and key partners as collaborators and co-creators in D&I studies.
- Studies on policy implementation, such as identifying effective strategies for implementing health-related policies across federal, state, local and organizational settings.
Key characteristics of dissemination and implementation (D&I) research that applicants could consider including in their applications (where applicable) include but are not limited to:
- Description and justification of the evidence-based intervention and hypothesized implementation strategies to improve implementation outcomes (e.g., acceptability, feasibility, adoption, fidelity, penetration, sustainability) as well as health service outcomes (e.g., quality, equity).
- Understanding of contextual factors that can influence dissemination or implementation of the evidence-based intervention in various settings under investigation
- Incorporation and justification of the use of D&I theories, models, and/or frameworks to inform study hypotheses, processes, measures, and outcomes.
- Consideration of the extant literature on barriers and facilitators, promising strategies, and/or putative mechanisms, of similar evidence-based interventions integrated in like settings.
- Identification of possible preconditions, mediators, moderators, and mechanisms of action that explain the impact of dissemination or implementation strategies on relevant outcomes.
- Consideration and characterization of the multi-level context and environment in which the proposed research will be conducted, including a description of the intended implementers.
- Consideration of the use of qualitative, mixed and/or multi methods approaches.
- Development and/or use of appropriate D&I related outcomes, measures, and analyses. Applicants are encouraged to review available resources and use standard measures and validated instruments where possible, rather than developing their own measures for each study.
- Attention to issues of resources expended, program costs, cost-effectiveness, or other economic outcomes related to dissemination and/or implementation.
- Incorporation of engagement science (i.e., engagement-related research questions), and including outcomes relevant to patients, consumers, families, practitioners, administrators, healthcare system leaders, and/or policymakers.
- Formation of multidisciplinary or transdisciplinary teams of researchers and implementing partners, given the range of expertise that may be needed for conducting dissemination and implementation research.
- Adequate consideration and specification of the equity-related approach and outcomes.
- Articulation of methods for tracking changes in context and/or adaptation of implementation strategies throughout the course of the study.
Non-responsive applications
- Applications that propose to test therapies, imaging, diagnostics, biologics, or devices (e.g., first-in-human studies or drug/device safety trials)
- Applications that propose to test an intervention in an efficacy trial
Information relevant to Specific Institutes/Centers
In addition to the above description of the scientific objectives, resources communicating scientific interests of selected Institutes and Centers (I/Cs) are summarized below. Applicants are encouraged to contact the Scientific/Research contact of the intended I/C to ensure that the aims of the proposed project are consistent with I/C mission.
National Cancer Institute (NCI)
NCI seeks implementation science projects across the cancer control continuum. Areas of interest include prevention, detection, and in areas less represented in the NCI-funded portfolio, including in cancer diagnosis, treatment, and survivorship. Examples include (but are not limited to) studies that seek to understand and evaluate sustainable approaches to coordinate cancer treatment across fragmented systems; optimizing survivorship care among oncology and non-oncology providers; and survivorship care delivery in diverse settings (e.g.,community practices, rural settings). Additionally, NCI is interested in supporting applications that focus on understanding strategies to promote sustainability and scale up of effective cancer control interventions, studies that seek to understand de-implementation, and studies that seek to advance measures and methods. Policy implementation research studies are encouraged.
NCI is interested in applications that seek to advance health equity through implementation science. Areas of interest include projects that promote equitable reach, delivery, and implementation of evidence-based interventions in/with communities and populations experiencing health disparities. To advance the equitable implementation, the NCI is interested in implementation strategies that incorporate social determinants of health or social needs in developing and testing strategies to advance adoption, adaptation, fidelity, acceptability, cost, and sustainability of evidence-based interventions in cancer prevention and control. Implementation research aims should be guided by equity-oriented theoretical models and frameworks and the equity related outcomes or approaches clearly described. Multilevel approaches and transdisciplinary and intersectoral collaborations (e.g., transportation, housing, food systems) are encouraged. To the extent possible, studies may include an evaluation to assess that implementation projects are not inadvertently exacerbating health disparities or inequalities. Research that engages public health practitioners in community settings (e.g., health departments, coalitions, community organizations) as well as practice-based research are encouraged.
In efforts to advance the field, NCI launched the Consortium for Cancer Implementation Science (CCIS) which broadly focuses on cancer control priorities, cross-collaborations across disciplines and institutions, and innovative solutions to advance measures and methods in implementation science. Applications that advance scientific priorities of the CCIS action groups are encouraged. See annual meeting summaries at: https://cancercontrol.cancer.gov/is/initiatives/ccis .
We encourage applicants to contact program staff for assistance early in the application process.
National Human Genome Research Institute (NHGRI)
NHGRI seeks implementation science projects that maximize the usability of genomics across the continuum of healthcare, public health, and society. NHGRI is interested in applications that develop and assess strategies for implementing the use of genomic information in clinical care, increase genomic literacy, and promote equitable access to and outcomes from genomic information. Strategies may include (but are not limited to) informatics strategies, alternate care models, and behavioral, social, and/or educational strategies. Multi-level approaches, transdisciplinary collaborations, and meaningful engagement of relevant communities (including clinical, familial, social, organizational) are encouraged.
To the extent possible, implementation studies should include evaluation to assess inadvertent exacerbation of inequities or disparities as well as how benefits may be experienced differently within the context of the implementation in order to further maximize health outcomes through genomic information. Applications for studies relevant only to a particular disease or organ system should be directed to the appropriate Institute or Center. NHGRI strongly encourages potential applicants to contact program staff in the early stages of developing your application.
Projects funded by NHGRI though this NOFO will be invited to join the Advancing Genomic Medicine Research (AGMR) Program. AGMR participants attend an annual AGMR Grantee Meeting hosted by NHGRI. These meetings serve as venues to facilitate sharing of research findings; promote the exchange of ideas; enable discussion of opportunities, challenges, and emerging needs; develop expertise and abilities among collaborators newer to genomic medicine; and accelerate progress in genomic medicine. Applicants to NHGRI through this NOFO may include in their budget travel costs to attend the annual AGMR Grantee Meetings in-person.
National Institute on Aging (NIA)
NIA is interested in research to identify and understand barriers to the adoption, adaptation, integration, scale-up, and sustainability of evidence-based health interventions, tools, and policies related to aging or older adults.
For clinical trial proposals, D&I strategies studied should be limited to strategies to disseminate and/or implement interventions that have evidence of efficacy/potency, as well as evidence that the intervention can be delivered in the community with fidelity. NIA is especially interested in receiving applications that fall within Stage V of the NIH Stage Model for Behavioral Intervention Development that focus on the mechanisms that promote the successful implementation and dissemination of interventions, consistent with the NIH Science of Behavior Change emphasis on mechanisms of change. Information about the NIH Stage Model for Behavioral Intervention Development can be found at: https://www.nia.nih.gov/research/dbsr/stage-model-behavioral-intervention-development . Information regarding NIH’s Science of Behavior Change (SOBC) program can be found at: https://commonfund.nih.gov/behaviorchange .
Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD)
The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) invites implementation science proposals that address questions relevant to the NICHD mission and align with the NICHD Strategic Plan . These include studies that aim to identify, develop and test innovative strategies that promote broad implementation, uptake and sustainability of interventions with proven efficacy and/or effectiveness. NICHD’s interests also include studies that test strategies aimed at de-implementing interventions that are harmful, non-cost-effective, ineffective, or lacking adequate scientific support.
Applications assigned to NICHD must address one or more NICHD priority populations. These include:
- Infants, children and adolescents, including individuals transitioning from pediatric to adult health care providers
- Pregnant, peripartum, postpartum and lactating persons
- Individuals of reproductive age with regards to gynecologic and reproductive health care
- Individuals of any age with intellectual and developmental disabilities
- Individuals of any age with physical disabilities
For more specific information on NICHD D&I priority research areas and staff contacts, please visit NICHD Priorities for Dissemination and Implementation Research . Applicants are encouraged to speak with an NICHD program official during concept development to discuss alignment with NICHD priorities. NOTE: Applications assigned to NICHD that address the mission and priorities of other institutes will not be prioritized for funding by NICHD.
National Institute of Dental and Craniofacial Research (NIDCR)
The NIDCR is interested in D&I research applications relevant to dental, oral, or craniofacial health that align with the NIDCR Strategic Plan. Investigators proposing research that meets the NIH definition of a clinical trial should refer to NIDCR Clinical Trials NOFOs. All investigators are encouraged to contact NIDCR Scientific/Research staff well before submission to discuss scientific priorities.
National Institute of Mental Health (NIMH)
The National Institute of Mental Health (NIMH) is interested in applications relevant to dissemination and implementation (D&I) research that support the NIMH Strategic Plan for Research . Because NIMH requires investigative teams to study the mechanisms underlying interventions (for instance, for drugs, devices and behavioral interventions directed at patients, NIMH requires the experimental therapeutics approach), all applications that propose clinical trials to test D&I strategies should go beyond assessing just whether a strategy is effective and should include hypotheses about how, why, for whom, and/or in what circumstances the strategy is effective. Potential approaches include but are not limited to mediation analyses (e.g., mediator mapping), moderator analysis, temporally organized dismantling designs, and partial or full factorial designs. For multi-component or multi-level strategies (e.g., approaches that combine multiple strategies to improve intervention reach, adoption, implementation, scalability, or sustainability of an intervention such as the Collaborative Care Model), other methods to examine the combined or dismantled effects of each of the components on the ultimate outcome(s) (versus modelling such effects through target/mediator variables) could also be employed, particularly if the study is adding a new component to enhance the effect of the combined strategy.
NIMH encourages a deployment-focused model of intervention design and testing that takes into account the perspective of relevant end-users (e.g., service users, providers, administrators, payers, policy makers) and the key characteristics of the settings (e.g., resources, including workforce capacity; existing clinical workflows). To this end NIMH strongly encourages meaningful inclusion of end-users in the research (e.g., member of an advisory panels and/or inclusion as key personnel). This attention to end-user perspectives is intended to help ensure the research findings will have clear utility to communities, practices, and/or policy makers who may benefit from those findings.
Adaptations or augmentations of existing implementation strategies should only be undertaken if there is (a) an empirical rationale for the adaptation/augmentation, (b) a clear hypothesis to understand how and why the adapted or augmented strategy will enhance outcomes, and (c) evidence to suggest that the adapted strategy will result in a substantial improvement in implementation outcomes (e.g. reach, adoption, scalability, sustainment) associated with the strategy and/or clinical or functional outcomes associated with the intervention. For more information, see https://www.nimh.nih.gov/funding/opportunities-announcements/clinical-trials-NOFOs
It is strongly encouraged that applicants contact NIMH program staff prior to submission to ensure that applicants are responsive to the institute’s priorities and criteria.
Fogarty International Center (FIC)
FIC aims to support research in low- and middle-income countries (LMICs), including through partnerships with US institutions and investigators, that will build and enhance the capacity of the LMIC institution(s) to carry out research in dissemination and implementation science. The proposed study should explore research capacity strengthening activities at the LMIC institution through structured activities or training. See also: FIC strategic plan https://www.fic.nih.gov/About/Pages/Strategic-Plan.aspx. For additional information regarding FIC supported implementation science research please refer to the following https://www.fic.nih.gov/ResearchTopics/Pages/ImplementationScience.aspx. All investigators are encouraged to contact FIC Scientific/Research staff prior to submission to discuss scientific priorities.
Tribal Health Research Office (THRO)
The Tribal Health Research Office (THRO) serves as the central point of contact at NIH for federally recognized American Indian and Alaska Native (AI/AN) Tribes throughout the United States (U.S.) and is the synergistic hub for all Tribal health research activities and research workforce development at NIH . The mission of THRO is to improve Native health, enhance capacity for health research in Native communities, and promote opportunities for the next generation of AI/AN researchers. THRO does not have grant-making authority or administer grants. The office can only support grants deemed scientifically meritorious after review by one of the institutes or centers (ICs) participating in this announcement and after a co-funding request is initiated through the IC.
For this NOFO, THRO is interested in supporting studies that develop and/or test strategies to overcome barriers to adoption, adaption, integration, scale-up and sustainability of evidence-based interventions, practices, programs, tools, treatments, guidelines, and policies in Tribal and/or American Indian/Alaska Native populations.
See Section VIII. Other Information for award authorities and regulations.
Plan for Enhancing Diverse Perspectives (PEDP)
The NIH recognizes that teams comprised of investigators with diverse perspectives working together and capitalizing on innovative ideas and distinct viewpoints outperform homogeneous teams. There are many benefits that flow from a scientific workforce rich with diverse perspectives, including: fostering scientific innovation, enhancing global competitiveness, contributing to robust learning environments, improving the quality of the research, advancing the likelihood that underserved populations participate in, and benefit from research, and enhancing public trust.
To support the best science, the NIH encourages inclusivity in research guided by the consideration of diverse perspectives. Broadly, diverse perspectives can include but are not limited to the educational background and scientific expertise of the people who perform the research; the populations who participate as human subjects in research studies; and the places where research is done.
This NOFO requires a Plan for Enhancing Diverse Perspectives (PEDP), which will be assessed as part of the scientific and technical peer review evaluation. Assessment of applications containing a PEDP are based on the scientific and technical merit of the proposed project. Consistent with federal law, the race, ethnicity, or sex of a researcher, award participant, or trainee will not be considered during the application review process or when making funding decisions. Applications that fail to include a PEDP will be considered incomplete and will be administratively withdrawn before review.
The PEDP will be submitted as Other Project Information as an attachment (see Section IV). Applicants are strongly encouraged to read the NOFO instructions carefully and view the available PEDP Guidance materials.
Section II. Award Information
Grant: A financial assistance mechanism providing money, property, or both to an eligible entity to carry out an approved project or activity.
The OER Glossary and the How to Apply Application Guide provide details on these application types. Only those application types listed here are allowed for this NOFO.
Not Allowed: Only accepting applications that do not propose clinical trials.
Need help determining whether you are doing a clinical trial?
The number of awards is contingent upon NIH appropriations and the submission of a sufficient number of meritorious applications.
A budget for direct costs of up to $50,000 per year may be requested.
The maximum project period is 2 years.
NIH grants policies as described in the NIH Grants Policy Statement will apply to the applications submitted and awards made from this NOFO.
Section III. Eligibility Information
1. eligible applicants eligible organizations higher education institutions public/state controlled institutions of higher education private institutions of higher education the following types of higher education institutions are always encouraged to apply for nih support as public or private institutions of higher education: hispanic-serving institutions historically black colleges and universities (hbcus) tribally controlled colleges and universities (tccus) alaska native and native hawaiian serving institutions asian american native american pacific islander serving institutions (aanapisis) nonprofits other than institutions of higher education nonprofits with 501(c)(3) irs status (other than institutions of higher education) nonprofits without 501(c)(3) irs status (other than institutions of higher education) for-profit organizations small businesses for-profit organizations (other than small businesses) local governments state governments county governments city or township governments special district governments indian/native american tribal governments (federally recognized) indian/native american tribal governments (other than federally recognized). federal governments eligible agencies of the federal government u.s. territory or possession other independent school districts public housing authorities/indian housing authorities native american tribal organizations (other than federally recognized tribal governments) faith-based or community-based organizations regional organizations non-domestic (non-u.s.) entities (foreign organizations) foreign organizations non-domestic (non-u.s.) entities (foreign organizations) are eligible to apply. non-domestic (non-u.s.) components of u.s. organizations are eligible to apply. foreign components, as defined in the nih grants policy statement , are allowed. required registrations applicant organizations applicant organizations must complete and maintain the following registrations as described in the how to apply- application guide to be eligible to apply for or receive an award. all registrations must be completed prior to the application being submitted. registration can take 6 weeks or more, so applicants should begin the registration process as soon as possible. failure to complete registrations in advance of a due date is not a valid reason for a late submission, please reference the nih grants policy statement section 2.3.9.2 electronically submitted applications for additional information. system for award management (sam) – applicants must complete and maintain an active registration, which requires renewal at least annually . the renewal process may require as much time as the initial registration. sam registration includes the assignment of a commercial and government entity (cage) code for domestic organizations which have not already been assigned a cage code. nato commercial and government entity (ncage) code – foreign organizations must obtain an ncage code (in lieu of a cage code) in order to register in sam. unique entity identifier (uei) - a uei is issued as part of the sam.gov registration process. the same uei must be used for all registrations, as well as on the grant application. era commons - once the unique organization identifier is established, organizations can register with era commons in tandem with completing their grants.gov registrations; all registrations must be in place by time of submission. era commons requires organizations to identify at least one signing official (so) and at least one program director/principal investigator (pd/pi) account in order to submit an application. grants.gov – applicants must have an active sam registration in order to complete the grants.gov registration. program directors/principal investigators (pd(s)/pi(s)) all pd(s)/pi(s) must have an era commons account. pd(s)/pi(s) should work with their organizational officials to either create a new account or to affiliate their existing account with the applicant organization in era commons. if the pd/pi is also the organizational signing official, they must have two distinct era commons accounts, one for each role. obtaining an era commons account can take up to 2 weeks. eligible individuals (program director/principal investigator) any individual(s) with the skills, knowledge, and resources necessary to carry out the proposed research as the program director(s)/principal investigator(s) (pd(s)/pi(s)) is invited to work with their organization to develop an application for support. individuals from diverse backgrounds, including underrepresented racial and ethnic groups, individuals with disabilities, and women are always encouraged to apply for nih support. see, reminder: notice of nih's encouragement of applications supporting individuals from underrepresented ethnic and racial groups as well as individuals with disabilities , not-od-22-019 and notice of nih's interest in diversity, not-od-20-031 . for institutions/organizations proposing multiple pds/pis, visit the multiple program director/principal investigator policy and submission details in the senior/key person profile (expanded) component of the how to apply-application guide. 2. cost sharing.
This NOFO does not require cost sharing as defined in the NIH Grants Policy Statement Section 1.2 Definition of Terms .
3. Additional Information on Eligibility
Number of Applications
Applicant organizations may submit more than one application, provided that each application is scientifically distinct.
The NIH will not accept duplicate or highly overlapping applications under review at the same time, per NIH Grants Policy Statement Section 2.3.7.4 Submission of Resubmission Application . This means that the NIH will not accept:
- A new (A0) application that is submitted before issuance of the summary statement from the review of an overlapping new (A0) or resubmission (A1) application.
- A resubmission (A1) application that is submitted before issuance of the summary statement from the review of the previous new (A0) application.
- An application that has substantial overlap with another application pending appeal of initial peer review (see NIH Grants Policy Statement 2.3.9.4 Similar, Essentially Identical, or Identical Applications ).
Section IV. Application and Submission Information
1. requesting an application package.
The application forms package specific to this opportunity must be accessed through ASSIST, Grants.gov Workspace or an institutional system-to-system solution. Links to apply using ASSIST or Grants.gov Workspace are available in Part 1 of this NOFO. See your administrative office for instructions if you plan to use an institutional system-to-system solution.
2. Content and Form of Application Submission
It is critical that applicants follow the instructions in the Research (R) Instructions in the How to Apply - Application Guide except where instructed in this notice of funding opportunity to do otherwise. Conformance to the requirements in the Application Guide is required and strictly enforced. Applications that are out of compliance with these instructions may be delayed or not accepted for review.
Page Limitations
All page limitations described in the How to Apply- Application Guide and the Table of Page Limits must be followed.
The following section supplements the instructions found in the How to Apply- Application Guide and should be used for preparing an application to this NOFO.
SF424(R&R) Cover
All instructions in the How to Apply - Application Guide must be followed.
SF424(R&R) Project/Performance Site Locations
All instructions in the How to Apply- Application Guide must be followed.
SF424(R&R) Other Project Information
- In an "Other Attachment" entitled "Plan for Enhancing Diverse Perspectives," all applicants must include a summary of actionable strategies to advance the scientific and technical merit of the proposed project through expanded inclusivity.
- Applicants should align their proposed strategies for PEDP with the research strategy section, providing a holistic and integrated view of how enhancing diverse perspectives and inclusivity are buoyed throughout the application.
- The PEDP will vary depending on the scientific aims, expertise required, the environment and performance site(s), as well as how the project aims are structured.
- Actionable strategies using defined approaches for the inclusion of diverse perspectives in the project;
- Description of how the PEDP will advance the scientific and technical merit of the proposed project;
- Anticipated timeline of proposed PEDP activities;
- Evaluation methods for assessing the progress and success of PEDP activities.
Examples of items that advance inclusivity in research and may be appropriate for a PEDP can include, but are not limited to:
- Partnerships with different types of institutions and organizations (e.g., research-intensive; undergraduate-focused; HBCUs; emerging research institutions; community-based organizations).
- Project frameworks that enable communities and researchers to work collaboratively as equal partners in all phases of the research process.
- Outreach and planned engagement activities to enhance recruitment of individuals from diverse groups as human subjects in clinical trials, including those from underrepresented backgrounds.
- Description of planned partnerships that may enhance geographic and regional diversity.
- Outreach and recruiting activities intended to diversify the pool of applicants for research training programs, such as outreach to prospective applicants from groups underrepresented in the biomedical sciences, for example, individuals from underrepresented racial and ethnic groups, those with disabilities, those from disadvantaged backgrounds, and women.
- Plans to utilize the project infrastructure (i.e., research and structure) to enhance the research environment and support career-advancing opportunities for junior, early- and mid-career researchers.
- Transdisciplinary research projects and collaborations among researchers from fields beyond the biological sciences, such as physics, engineering, mathematics, computational biology, computer and data sciences, as well as bioethics.
Examples of items that are not appropriate in a PEDP include, but are not limited to:
- Selection or hiring of personnel for a research team based on their race, ethnicity, or sex.
- A training or mentorship program limited to certain researchers based on their race, ethnicity, or sex.
For further information on the Plan for Enhancing Diverse Perspectives (PEDP), please see PEDP Guidance materials.
SF424(R&R) Senior/Key Person Profile
R&r or modular budget.
PEDP implementation costs: Applicants may include allowable costs associated with PEDP implementation (as outlined in the Grants Policy Statement section 7): https://grants.nih.gov/grants/policy/nihgps/html5/section_7/7.1_general.htm.
R&R Subaward Budget
All instructions in the How to Apply-Application Guide must be followed.
PHS 398 Cover Page Supplement
Phs 398 research plan.
All instructions in the How to Apply- Application Guide must be followed, with the following additional instructions:
Research Strategy: The Research Strategy should clearly describe the following within the appropriate section (i.e., Factor 1: Importance of the Research; Factor 2: Rigor and Feasibility; Factor 3: Expertise and Resources):
Factor 1: Importance of the Research (Significance, Innovation)
- The estimated public health benefit of the research, and whether the existing data, public health and patient needs justify dissemination and implementation.
- If the aims of the proposed project are achieved, how the study results will advance dissemination and implementation knowledge. The ability of potential adopters and organizations to determine the applicability of the results to their setting.
- The reach (to the population that will benefit from the knowledge/intervention) that will be achieved and the equitability of the reach and likely outcomes through the knowledge/service delivery contexts selected.
- How the proposed dissemination or implementation research contributes new and innovative concepts, outcomes, measures, and/or design approaches to the field.
- How the study proposed promises to speed the translation of research into practice and/or produce novel and robust findings.
Factor 2: Rigor and Feasibility (Approach)
- Demonstrate an understanding of dissemination and implementation research principles. How the dissemination or implementation approach is appropriate to the problem and population using research methods that are relevant, rigorous and practical.
- Justify the study design on the basis of the current state-of-the-art and or contextual factors relevant to dissemination and/or implementation.
- How the procedures to assess and analyze the dissemination or implementation strategies are appropriate.
- How the measurements and analysis plan are linked to the study aims, and whether the analysis incorporates the best available data to track dissemination or implementation process and impact, including cost-effectiveness.
- Where applicable, how the proposed plan for analysis takes into account hierarchical relationships among multiple levels of outcomes (e.g. patient/consumer, provider, system).
Factor 3: Expertise and Resources (Investigators, Environment)
- Whether the investigators are part of stakeholder teams or have strong links and engagement of stakeholders necessary to accomplish the project aims.
- Clear evidence of dissemination and implementation research expertise as part of the team.
- How the proposed approaches take advantage of unique features of the intervention delivery environment or employ useful, collaborative arrangements
Letters of Support: the letters of collaboration and institutional support should include the level of commitment to the project.
Resource Sharing Plan : Individuals are required to comply with the instructions for the Resource Sharing Plans as provided in the How to Apply- Application Guide.
- All applications, regardless of the amount of direct costs requested for any one year, should address a Data Sharing Plan.
Other Plan(s):
All instructions in the How to Apply-Application Guide must be followed, with the following additional instructions:
- All applicants planning research (funded or conducted in whole or in part by NIH) that results in the generation of scientific data are required to comply with the instructions for the Data Management and Sharing Plan. All applications, regardless of the amount of direct costs requested for any one year, must address a Data Management and Sharing Plan.
Appendix: Only limited Appendix materials are allowed. Follow all instructions for the Appendix as described in the How to Apply- Application Guide.
- No publications or other material, with the exception of blank questionnaires or blank surveys, may be included in the Appendix.
PHS Human Subjects and Clinical Trials Information
When involving human subjects research, clinical research, and/or NIH-defined clinical trials (and when applicable, clinical trials research experience) follow all instructions for the PHS Human Subjects and Clinical Trials Information form in the How to Apply- Application Guide, with the following additional instructions:
If you answered “Yes” to the question “Are Human Subjects Involved?” on the R&R Other Project Information form, you must include at least one human subjects study record using the Study Record: PHS Human Subjects and Clinical Trials Information form or Delayed Onset Study record.
Study Record: PHS Human Subjects and Clinical Trials Information
Delayed Onset Study
Note: Delayed onset does NOT apply to a study that can be described but will not start immediately (i.e., delayed start).All instructions in the How to Apply- Application Guide must be followed.
PHS Assignment Request Form
Foreign organizations.
Foreign (non-U.S.) organizations must follow policies described in the NIH Grants Policy Statement , and procedures for foreign organizations described throughout the How to Apply- Application Guide.
3. Unique Entity Identifier and System for Award Management (SAM)
See Part 2. Section III.1 for information regarding the requirement for obtaining a unique entity identifier and for completing and maintaining active registrations in System for Award Management (SAM), NATO Commercial and Government Entity (NCAGE) Code (if applicable), eRA Commons, and Grants.gov
4. Submission Dates and Times
Part I. contains information about Key Dates and times. Applicants are encouraged to submit applications before the due date to ensure they have time to make any application corrections that might be necessary for successful submission. When a submission date falls on a weekend or Federal holiday , the application deadline is automatically extended to the next business day.
Organizations must submit applications to Grants.gov (the online portal to find and apply for grants across all Federal agencies). Applicants must then complete the submission process by tracking the status of the application in the eRA Commons , NIH’s electronic system for grants administration. NIH and Grants.gov systems check the application against many of the application instructions upon submission. Errors must be corrected and a changed/corrected application must be submitted to Grants.gov on or before the application due date and time. If a Changed/Corrected application is submitted after the deadline, the application will be considered late. Applications that miss the due date and time are subjected to the NIH Grants Policy Statement Section 2.3.9.2 Electronically Submitted Applications .
Applicants are responsible for viewing their application before the due date in the eRA Commons to ensure accurate and successful submission.
Information on the submission process and a definition of on-time submission are provided in the How to Apply-Application Guide.
5. Intergovernmental Review (E.O. 12372)
This initiative is not subject to intergovernmental review.
6. Funding Restrictions
All NIH awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Pre-award costs are allowable only as described in the NIH Grants Policy Statement Section 7.9.1 Selected Items of Cost.
Applications must be submitted electronically following the instructions described in the How to Apply - Application Guide . Paper applications will not be accepted.
Applicants must complete all required registrations before the application due date. Section III. Eligibility Information contains information about registration.
For assistance with your electronic application or for more information on the electronic submission process, visit How to Apply – Application Guide . If you encounter a system issue beyond your control that threatens your ability to complete the submission process on-time, you must follow the Dealing with System Issues guidance. For assistance with application submission, contact the Application Submission Contacts in Section VII .
Important reminders:
All PD(s)/PI(s) must include their eRA Commons ID in the Credential field of the Senior/Key Person Profile form . Failure to register in the Commons and to include a valid PD/PI Commons ID in the credential field will prevent the successful submission of an electronic application to NIH. See Section III of this NOFO for information on registration requirements.
The applicant organization must ensure that the unique entity identifier provided on the application is the same identifier used in the organization’s profile in the eRA Commons and for the System for Award Management. Additional information may be found in the How to Apply - Application Guide .
See more tips for avoiding common errors.
Applications must include a PEDP submitted as Other Project Information as an attachment. Applications that fail to include a PEDP will be considered incomplete and will be administratively withdrawn before review.
Upon receipt, applications will be evaluated for completeness and compliance with application instructions by the Center for Scientific Review, NIH. Applications that are incomplete or non-compliant will not be reviewed.
Recipients or subrecipients must submit any information related to violations of federal criminal law involving fraud, bribery, or gratuity violations potentially affecting the federal award. See Mandatory Disclosures, 2 CFR 200.113 and NIH Grants Policy Statement Section 4.1.35 .
Send written disclosures to the NIH Chief Grants Management Officer listed on the Notice of Award for the IC that funded the award and to the HHS Office of Inspector Grant Self Disclosure Program at [email protected] .
Post Submission Materials
Applicants are required to follow the instructions for post-submission materials, as described in the policy
Section V. Application Review Information
1. criteria.
Only the review criteria described below will be considered in the review process. Applications submitted to the NIH in support of the NIH mission are evaluated for scientific and technical merit through the NIH peer review system.
Reviewers will provide an overall impact score to reflect their assessment of the likelihood for the project to exert a sustained, powerful influence on the research field(s) involved, in consideration of the following scored review criteria and additional review criteria (as applicable for the project proposed). An application does not need to be strong in all categories to be judged likely to have a major scientific impact. As part of the overall impact score, reviewers should consider and indicate how the Plan for Enhancing Diverse Perspectives affects the scientific merit of the project.
Reviewers will evaluate Factors 1, 2 and 3 in the determination of scientific merit, and in providing an overall impact score. In addition, Factors 1 and 2 will each receive a separate criterion score.
Significance
- Evaluate the importance of the proposed research in the context of current scientific challenges and opportunities, either for advancing knowledge within the field, or more broadly. Assess whether the application addresses an important gap in knowledge in the field, would solve a critical problem, or create a valuable conceptual or technical advance.
- Evaluate the rationale for undertaking the study, the rigor of the scientific background for the work (e.g., prior literature and/or preliminary data) and whether the scientific background justifies the proposed study.
- Evaluate the extent to which innovation influences the importance of undertaking the proposed research. Note that while technical or conceptual innovation can influence the importance of the proposed research, a project that is not applying novel concepts or approaches may be of critical importance for the field.
- Evaluate whether the proposed work applies novel concepts, methods or technologies or uses existing concepts, methods, technologies in novel ways, to enhance the overall impact of the project.
Specific to this NOFO:
- Evaluate the extent to which the existing data, public health, and patient needs justify dissemination and implementation
- Evaluate whether the study would advance knowledge in dissemination and implementation if the proposed aims are achieved
- Evaluate the degree to which the study contexts are likely to inform equitable reach (to the population that will benefit from the knowledge/intervention) and outcomes
- Evaluate whether consideration has been given to resource requirements and costs of the intervention
- Evaluate whether potential adopters and organizations will be able to determine the applicability of the results to their settings
- Evaluate whether the study holds promise for speeding the translation of research into practice or policy
- Evaluate the scientific quality of the proposed work. Evaluate the likelihood that compelling, reproducible findings will result (rigor) and assess whether the proposed studies can be done well and within the timeframes proposed (feasibility).
- Evaluate the potential to produce unbiased, reproducible, robust data.
- Evaluate the rigor of experimental design and whether appropriate controls are in place.
- Evaluate whether the sample size is sufficient and well-justified.
- Assess the quality of the plans for analysis, interpretation, and reporting of results.
- Evaluate whether the investigators presented adequate plans to address relevant biological variables, such as sex or age, in the design, analysis, and reporting.
- the rigor of the intervention or study manipulation (if applicable to the study design).
- whether outcome variables are justified.
- whether the results will be generalizable or, in the case of a rare disease/special group, relevant to the particular subgroup.
- whether the sample is appropriate and sufficiently diverse to address the proposed question(s).
- For applications involving human subjects, including clinical trials, assess the adequacy of inclusion plans as appropriate for the scientific goals of the research. Considerations of appropriateness may include disease/condition/behavior incidence, prevalence, or population burden, population representation, and/or current state of the science.
Feasibility:
- Evaluate whether the proposed approach is sound and achievable, including plans to address problems or new challenges that emerge in the work. For proposed studies in which feasibility may be less certain, evaluate whether the uncertainty is balanced by the potential for major advances.
- For applications involving human subjects, including clinical trials, evaluate the adequacy and feasibility of the plan to recruit and retain an appropriately diverse population of participants. Additionally, evaluate the likelihood of successfully achieving the proposed enrollment based on age, racial, ethnic, and sex/gender categories.
- For clinical trial applications, evaluate whether the study timeline and milestones are feasible.
- Evaluate whether the applicant demonstrates an understanding of dissemination and implementation research principles
- Evaluate whether the applicant justified the study design on the basis of current state-of-the-art and/or contextual factors relevant to dissemination and implementation
- Evaluate whether the dissemination or implementation approach is appropriate to the problem and population using, research methods that are relevant, rigorous, and practical
- Evaluate whether the procedures to assess and analyze the dissemination or implementation strategies are appropriate
- Evaluate whether the measurements and analysis plan are linked to the study aims and incorporate the best available data to track dissemination or implementation process and impact, including cost-effectiveness.
- Evaluate, where applicable, whether the proposed plan for analysis takes into account hierarchical relationships among multiple levels of outcomes (e.g., patient, provider, system)
Investigator(s)
Evaluate whether the investigator(s) have demonstrated background, training, and expertise, as appropriate for their career stage, to conduct the proposed work. For Multiple Principal Investigator (MPI) applications, assess the quality of the leadership plan to facilitate coordination and collaboration.
Environment
Evaluate whether the institutional resources are appropriate to ensure the successful execution of the proposed work.
- Evaluate whether the investigators are part of stakeholder teams or have strong links and engagement of stakeholders necessary to accomplish the project aims
- Evaluate whether there is clear evidence of dissemination and implementation research expertise as part of the team
As applicable for the project proposed, reviewers will consider the following additional items while determining scientific and technical merit, but will not give criterion scores for these items, and should consider them in providing an overall impact score.
For research that involves human subjects but does not involve one of the categories of research that are exempt under 45 CFR Part 46, evaluate the justification for involvement of human subjects and the proposed protections from research risk relating to their participation according to the following five review criteria: 1) risk to subjects; 2) adequacy of protection against risks; 3) potential benefits to the subjects and others; 4) importance of the knowledge to be gained; and 5) data and safety monitoring for clinical trials.
For research that involves human subjects and meets the criteria for one or more of the categories of research that are exempt under 45 CFR Part 46, evaluate: 1) the justification for the exemption; 2) human subjects involvement and characteristics; and 3) sources of materials. For additional information on review of the Human Subjects section, please refer to the Guidelines for the Review of Human Subjects .
When the proposed research includes Vertebrate Animals, evaluate the involvement of live vertebrate animals according to the following criteria: (1) description of proposed procedures involving animals, including species, strains, ages, sex, and total number to be used; (2) justifications for the use of animals versus alternative models and for the appropriateness of the species proposed; (3) interventions to minimize discomfort, distress, pain and injury; and (4) justification for euthanasia method if NOT consistent with the AVMA Guidelines for the Euthanasia of Animals. For additional information on review of the Vertebrate Animals section, please refer to the Worksheet for Review of the Vertebrate Animals Section .
When the proposed research includes Biohazards, evaluate whether specific materials or procedures that will be used are significantly hazardous to research personnel and/or the environment, and whether adequate protection is proposed.
As applicable, evaluate the full application as now presented.
As applicable, evaluate the progress made in the last funding period.
As applicable, evaluate the appropriateness of the proposed expansion of the scope of the project.
As applicable for the project proposed, reviewers will consider each of the following items, but will not give scores for these items, and should not consider them in providing an overall impact score.
For projects involving key biological and/or chemical resources, evaluate the brief plans proposed for identifying and ensuring the validity of those resources.
Evaluate whether the budget and the requested period of support are fully justified and reasonable in relation to the proposed research.
2. Review and Selection Process Applications will be evaluated for scientific and technical merit by (an) appropriate Scientific Review Group(s) convened by{LOCUS OF REVIEW}, in accordance with NIH peer review policy and procedures , using the stated review criteria . Assignment to a Scientific Review Group will be shown in the eRA Commons. As part of the scientific peer review, all applications will receive a written critique. Applications may undergo a selection process in which only those applications deemed to have the highest scientific and technical merit (generally the top half of applications under review) will be discussed and assigned an overall impact score. Applications will be assigned on the basis of established PHS referral guidelines to the appropriate NIH Institute or Center. Applications will compete for available funds with all other recommended applications submitted in response to this NOFO. Following initial peer review, recommended applications will receive a second level of review by the appropriate national Advisory Council or Board. The following will be considered in making funding decisions, consistent with applicable law. Scientific and technical merit of the proposed project, including the PEDP, as determined by scientific peer review. Availability of funds. Relevance of the proposed project to program priorities. Please note that reviewers will not consider race, ethnicity, age, or gender of a researcher, award participant, or trainee, even in part, in providing critiques, scores, or funding recommendations. NIH will not consider such factors in making its funding decisions. If the application is under consideration for funding, NIH will request "just-in-time" information from the applicant as described in the NIH Grants Policy Statement Section 2.5.1. Just-in-Time Procedures . This request is not a Notice of Award nor should it be construed to be an indicator of possible funding. Prior to making an award, NIH reviews an applicant’s federal award history in SAM.gov to ensure sound business practices. An applicant can review and comment on any information in the Responsibility/Qualification records available in SAM.gov. NIH will consider any comments by the applicant in the Responsibility/Qualification records in SAM.gov to ascertain the applicant’s integrity, business ethics, and performance record of managing Federal awards per 2 CFR Part 200.206 “Federal awarding agency review of risk posed by applicants.” This provision will apply to all NIH grants and cooperative agreements except fellowships. 3. Anticipated Announcement and Award Dates
After the peer review of the application is completed, the PD/PI will be able to access his or her Summary Statement (written critique) via the eRA Commons . Refer to Part 1 for dates for peer review, advisory council review, and earliest start date.
Information regarding the disposition of applications is available in the NIH Grants Policy Statement Section 2.4.4 Disposition of Applications .
Section VI. Award Administration Information
1. award notices.
A Notice of Award (NoA) is the official authorizing document notifying the applicant that an award has been made and that funds may be requested from the designated HHS payment system or office. The NoA is signed by the Grants Management Officer and emailed to the recipient’s business official.
In accepting the award, the recipient agrees that any activities under the award are subject to all provisions currently in effect or implemented during the period of the award, other Department regulations and policies in effect at the time of the award, and applicable statutory provisions.
Recipients must comply with any funding restrictions described in Section IV.6. Funding Restrictions . Any pre-award costs incurred before receipt of the NoA are at the applicant's own risk. For more information on the Notice of Award, please refer to the NIH Grants Policy Statement Section 5. The Notice of Award and NIH Grants & Funding website, see Award Process.
Institutional Review Board or Independent Ethics Committee Approval: Recipient institutions must ensure that protocols are reviewed by their IRB or IEC. To help ensure the safety of participants enrolled in NIH-funded studies, the recipient must provide NIH copies of documents related to all major changes in the status of ongoing protocols.
2. Administrative and National Policy Requirements
The following Federal wide and HHS-specific policy requirements apply to awards funded through NIH:
- The rules listed at 2 CFR Part 200 , Uniform Administrative Requirements, Cost Principles, and Audit Requirements for Federal Awards.
- All NIH grant and cooperative agreement awards include the NIH Grants Policy Statement as part of the terms and conditions in the Notice of Award (NoA). The NoA includes the requirements of this NOFO. For these terms of award, see the NIH Grants Policy Statement Part II: Terms and Conditions of NIH Grant Awards, Subpart A: General and Part II: Terms and Conditions of NIH Grant Awards, Subpart B: Terms and Conditions for Specific Types of Grants, Recipients, and Activities .
- HHS recognizes that NIH research projects are often limited in scope for many reasons that are nondiscriminatory, such as the principal investigator’s scientific interest, funding limitations, recruitment requirements, and other considerations. Thus, criteria in research protocols that target or exclude certain populations are warranted where nondiscriminatory justifications establish that such criteria are appropriate with respect to the health or safety of the subjects, the scientific study design, or the purpose of the research. For additional guidance regarding how the provisions apply to NIH grant programs, please contact the Scientific/Research Contact that is identified in Section VII under Agency Contacts of this NOFO.
All federal statutes and regulations relevant to federal financial assistance, including those highlighted in NIH Grants Policy Statement Section 4 Public Policy Requirements, Objectives and Other Appropriation Mandates.
Recipients are responsible for ensuring that their activities comply with all applicable federal regulations. NIH may terminate awards under certain circumstances. See 2 CFR Part 200.340 Termination and NIH Grants Policy Statement Section 8.5.2 Remedies for Noncompliance or Enforcement Actions: Suspension, Termination, and Withholding of Support .
Consistent with the 2023 NIH Policy for Data Management and Sharing, when data management and sharing is applicable to the award, recipients will be required to adhere to the Data Management and Sharing requirements as outlined in the NIH Grants Policy Statement . Upon the approval of a Data Management and Sharing Plan, it is required for recipients to implement the plan as described.
4. Reporting
When multiple years are involved, recipients will be required to submit the Research Performance Progress Report (RPPR) annually and financial statements as required in the NIH Grants Policy Statement Section 8.4.1 Reporting. To learn more about post-award monitoring and reporting, see the NIH Grants & Funding website, see Post-Award Monitoring and Reporting .
- Awardees will provide updates at least annually on implementation of the PEDP.
A final RPPR, invention statement, and the expenditure data portion of the Federal Financial Report are required for closeout of an award, as described in the NIH Grants Policy Statement Section 8.6 Closeout . NIH NOFOs outline intended research goals and objectives. Post award, NIH will review and measure performance based on the details and outcomes that are shared within the RPPR, as described at 2 CFR Part 200.301.
Enter text here.
Section VII. Agency Contacts
We encourage inquiries concerning this funding opportunity and welcome the opportunity to answer questions from potential applicants.
eRA Service Desk (Questions regarding ASSIST, eRA Commons, application errors and warnings, documenting system problems that threaten submission by the due date, and post-submission issues)
Finding Help Online: https://www.era.nih.gov/need-help (preferred method of contact) Telephone: 301-402-7469 or 866-504-9552 (Toll Free)
General Grants Information (Questions regarding application instructions, application processes, and NIH grant resources) Email: [email protected] (preferred method of contact) Telephone: 301-480-7075
Grants.gov Customer Support (Questions regarding Grants.gov registration and Workspace) Contact Center Telephone: 800-518-4726 Email: [email protected]
Gila Neta, PhD National Cancer Institute (NCI) Telephone: 240-276-6785 Email: [email protected]
Lori Ducharme NIDA - NATIONAL INSTITUTE ON DRUG ABUSE Phone: 301-827-6331 E-mail: [email protected]
Elizabeth L. Neilson, PhD, MPH, MSN Office of Disease Prevention (ODP) Phone: 301-827-5578 Email: [email protected]
Mary Acri, Ph.D. National Institute of Mental Health (NIMH) Telephone: 301-910-8230 Email: [email protected]
Tracy M. King, MD, MPH Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Telephone: 301-402-1822 Email: [email protected]
Alanna Kulchak Rahm, PhD, MS, CGC NHGRI - NATIONAL HUMAN GENOME RESEARCH INSTITUTE Phone: none E-mail: [email protected]
Jill Mattia, PhD Director, Assessment, Technology, and Treatment Outcomes Research Program National Institute of Dental and Craniofacial Research (NIDCR) (301) 451-7770 E-mail: [email protected]
Lisa Onken, Ph.D. Division of Behavioral and Social Research (DBSR) National Institute on Aging (NIA) Phone: 30l- 496-3131 E-mail: [email protected]
Richard T Benson NINDS - NATIONAL INSTITUTE OF NEUROLOGICAL DISORDERS AND STROKE Phone: 301-496-9135 E-mail: [email protected]
Claudia Thompson, Ph.D. NIEHS - National Institute of Environment Health Sciences Phone: (984) 287-3330 E-mail: [email protected]
Laura Kwako, Ph.D. National Institute on Alcohol Abuse and Alcoholism (NIAAA) Telephone: 301-451-8507 Email: [email protected]
Marya Levintova FIC - FOGARTY INTERNATIONAL CENTER Phone: 301-496-1653 E-mail: [email protected]
Sheila Caldwell, PhD Tribal Health Research Office Phone: 301-480-3527 email: [email protected]
Examine your eRA Commons account for review assignment and contact information (information appears two weeks after the submission due date).
Crystal Wolfrey National Cancer Institute ( NCI ) Telephone: 301-496-8634 Email: [email protected]
Bruce R Butrum Fogarty International Center (FIC) Telephone: 301-451-6830 E-mail: [email protected]
Deanna L Ingersoll National Human Genome Research Institute (NHGRI) Telephone: 301-435-7858 E-mail: [email protected]
Judy Fox National Institute on Alcohol Abuse and Alcoholism (NIAAA) Telephone: 301-443-4707 Email: [email protected]
Jenny L Greer National Institute of Environmental Health Sciences (NIEHS) Telephone: 984.287.3332 E-mail: [email protected]
Pamela G Fleming National Institute on Drug Abuse (NIDA) Telephone: 301-480-1159 E-mail: [email protected]
Tamara Kees National Institute of Mental Health (NIMH) Telephone: 301-443-8811 Email: [email protected]
Ryan Blakeney National Institute on Aging (NIA) Telephone: 301-451-9802 E-mail: [email protected]
Chief Grants Management Officer National Institute of Neurological Disorders and Stroke (NINDS) Email: [email protected]
Margaret Young Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Telephone: 301-642-4552 Email: [email protected]
Gabriel Hidalgo, MBA NIDCR - NATIONAL INSTITUTE OF DENTAL & CRANIOFACIAL RESEARCH Phone: 301-827-4630 E-mail: [email protected]
Section VIII. Other Information
Recently issued trans-NIH policy notices may affect your application submission. A full list of policy notices published by NIH is provided in the NIH Guide for Grants and Contracts . All awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Awards are made under the authorization of Sections 301 and 405 of the Public Health Service Act as amended (42 USC 241 and 284) and under Federal Regulations 42 CFR Part 52 and 2 CFR Part 200.

Dissemination as Dialogue: Building Trust and Sharing Research Findings Through Community Engagement
TOOLS AND TECHNIQUES — Volume 13 — March 17, 2016
Bryce McDavitt, PhD; Laura M. Bogart, PhD; Matt G. Mutchler, PhD; Glenn J. Wagner, PhD; Harold D. Green Jr, PhD; Sean Jamar Lawrence; Kieta D. Mutepfa, MSW; Kelsey A. Nogg
Suggested citation for this article: McDavitt B, Bogart LM, Mutchler MG, Wagner GJ, Green HD Jr, Lawrence SJ, et al. Dissemination as Dialogue: Building Trust and Sharing Research Findings Through Community Engagement. Prev Chronic Dis 2016;13:150473. DOI: http://dx.doi.org/10.5888/pcd13.150473 external icon .
PEER REVIEWED
Introduction
Planning a community dissemination phase, reaching out to community partners, tailoring content for various audiences, sharing the findings and building trust, deepening trust through ongoing dialogue, acknowledgments, author information.
A fundamental feature of community-based participatory research (CBPR) is sharing findings with community members and engaging community partners in the dissemination process. To be truly collaborative, dissemination should involve community members in a two-way dialogue about new research findings. Yet little literature describes how to engage communities in dialogue about research findings, especially with historically marginalized communities where mistrust of researchers may exist because of past or present social injustices. Through a series of interactive community presentations on findings from a longitudinal study, we developed a process for community dissemination that involved several overlapping phases: planning, outreach, content development, interactive presentations, and follow-up. Through this process, we built on existing and new community relationships. Following each interactive presentation, the research team debriefed and reviewed notes to identify lessons learned from the process. Key themes included the importance of creating a flexible dissemination plan, tailoring presentations to each community group, establishing a point person to serve as a community liaison, and continuing dialogue with community members after the presentations. Core strategies for developing trust during dissemination included engaging community members at every step, reserving ample time for discussion during presentations, building rapport by sharing personal experiences, being receptive to and learning from criticism, and implementing input from community members. This process led to a deeper understanding of research findings and ensured that results reached community members who were invested in them.
Sharing research findings with community members is a vital component of community-based participatory research (CBPR) for several reasons (1,2). First, community members deserve access to the knowledge they have made possible through participation or other forms of engagement in a study (3). Second, community dissemination creates opportunities to explore the implications of research findings from a local perspective (4). Third, dissemination allows providers to implement findings immediately and locally (5), potentially reducing the gap between research and practice (6). Finally, by fostering dialogue with those most affected by a given health issue, community dissemination aids in developing culturally relevant interventions (7).
Involving community members in discussions about new findings is particularly crucial for addressing health disparities. Those who work with or are members of a target population can shed light on factors that need to be addressed (8,9); without such input interventions may be ineffective. For example, although research has identified culturally specific determinants of treatment adherence among black people living with human immunodeficiency virus (HIV) (10–13), interventions to improve adherence have rarely been tailored for this population; this lack of tailoring may account for the comparatively weak effects found in adherence intervention trials that have a substantial number of black participants (14–16). Unless health care providers and other community members are engaged in collaborative partnerships to generate insights about research findings, opportunities to render interventions responsive to culturally specific determinants may be missed.
To foster partnerships, community dissemination should involve “a two-way dialogue, not a one-way flow of information” (17). Two-way dissemination enables community interpretations of findings to be integrated as part of an iterative research process (5), and it is more likely to influence health care practice than unidirectional dissemination (6). However, the CBPR dissemination literature primarily emphasizes passive, unidirectional dissemination strategies (eg, press releases, policy briefs, newsletters, websites). Apart from brief allusions to workshops with community members (3,18,19), scant literature examines how to implement community dissemination as a two-way dialogue or address its challenges, which may include translating research terminology into lay language (20), and — when findings focus on historically marginalized communities — how to discuss research in ways that are sensitive to mistrust and concerns about being stigmatized (21–23).
This article presents lessons learned from implementing community dissemination through a series of interactive community presentations. We discuss strategies for facilitating two-way dialogue and developing trust with communities to strengthen partnerships, gain a better understanding of findings, and explore implications for culturally relevant interventions and public policy.
The study and the Community Advisory Board. Project Mednet was a longitudinal study that examined how social network characteristics are associated with health outcomes and behaviors of black men and women living with HIV (24). The study was based on CBPR principles and conducted in partnership with AIDS Project Los Angeles (APLA), a large community-based organization (CBO) with an on-site co-investigator (M.G.M.) and an in-house research program with a community advisory board (CAB). We approach CBPR as a process grounded in working relationships sustained over time rather than convened for individual studies. For example, in addition to holding an academic post, the on-site co-investigator has been employed by APLA for more than 15 years, which has enabled him to develop and strengthen trusting relationships with many local providers and clients. The CAB has been sustained across multiple studies, and it comprises 6 clients and 12 service providers from 4 local social service agencies and 4 community clinics that primarily serve black people living with HIV. The service providers include HIV treatment educators, social workers, outreach staff, and HIV/AIDS clinicians. Sixteen CAB members are black, one is white, and one is Latino. For Project Mednet, CAB members provided guidance on study planning, data collection, analysis, and dissemination, including the decision to conduct a series of interactive presentations as a core community dissemination strategy. It was also important to the team and the CAB that the research team include members of the population being engaged and that staff were hired from the local community.
The community dissemination process. We conceptualized community dissemination as an ongoing dialogue with the community involving several overlapping phases: 1) planning, 2) outreach, 3) content development, 4) presentations with discussions, and 5) follow-up. Interactive presentations were conducted during a 6-month period, concurrent with evaluation of the process with CAB members, reinterpretation of data, and revision of presentation structure and content. Eleven presentations were conducted, with an average of 20 attendees per event. Presentation venues included 3 standing community meetings of service providers and clients, such as the Los Angeles Commission on HIV. Three were held for clients at CBOs, such as an agency that provides addiction counseling and health education to black men living with HIV. Two were held for staff at CBOs, including APLA, where most of the data were collected. One presentation was conducted as continuing education training for nurses and physicians who work primarily with black people living with HIV in South Los Angeles. Finally, 2 smaller presentations were conducted for leadership at 2 CBOs that had expressed interest in the findings: a national think tank that advocates for black people living with HIV and a grass-roots organization that provides wellness-oriented social activities for people living with HIV.
Identifying lessons learned. Throughout the dissemination phase, notes were collected on the interactive presentations, including content of discussions, challenges encountered, and input on findings or the dissemination process itself. During CAB meetings and in research team debriefing sessions after the presentations, preliminary themes were identified and strategies to refine the dissemination process were developed. This process continued throughout the dissemination phase, including during later small-group meetings with community providers to identify targeted strategies for implementing findings within existing programs or upcoming grant proposals.
Build community dissemination into project aims. A main study aim was to share findings with community stakeholders and, with their input, to identify novel intervention solutions to address medical mistrust and support adherence among black people living with HIV. Establishing this aim in the grant proposal made presentations a priority and fostered a sense of accountability among research team members. Having presentations as a formal aim also allowed us to budget funds for protected staff time to implement community dissemination. We found that funds were needed to cover staff time at multiple levels so that the research team could develop and maintain relationships with community members and CBOs. The principal investigator (L.M.B.) needed time to prepare and lead interactive presentations and engage in one-on-one communication with community members. Given her role as the research team leader, her active involvement was appreciated by community members because it demonstrated the value we placed on their input. The study coordinator (B.M.) was responsible for reaching out to CBOs, maintaining relationships, revising slide sets, coordinating logistics, conducting presentations, and facilitating discussions. A research assistant (K.A.N.) collected notes on discussions. A co-investigator (M.G.M.) also conducted interactive presentations, and an interviewer (S.J.L.) presented the study methods. Because we mainly held in-person presentations at standing meetings, expenditures for printing and space rental were minimal. However, at some presentations funds were needed for refreshments, which allowed clients and staff to attend during lunch breaks.
Develop a plan with community members, but keep it flexible. In collaboration with the CAB we developed an initial plan for dissemination, but because community partnerships should be flexible (25), our plan evolved iteratively in response to community feedback throughout the process. In addition to holding brainstorming sessions during CAB meetings on how to disseminate findings, we had in-depth conversations with key CAB members. We selected interactive presentations as our core dissemination strategy to create opportunities to engage community members in two-way dialogue. The research team and CAB developed a preliminary list of local venues and CBOs whose staff or clients might be interested in the findings, starting with CBOs where data had been collected or who had referred participants to us; this list evolved as new opportunities arose.
Presenting at standing meetings is often more practical than planning special events. Initially we considered conducting multi-hour Project Mednet public forums, but this approach was often impractical given the busy schedules of CBO staff members. CAB members suggested that instead we integrate our presentations into standing meetings, such as CBO staff meetings, continuing education trainings, or community forums where clients and staff from multiple CBOs gathered regularly. This approach resulted in strong attendance and produced in-depth discussions with a diverse range of groups, such as nurses working with people living with HIV or young gay men of color attending an HIV education program. We found that coordinators of many standing meetings were actively searching for relevant and timely content and that providing content for these meetings was a valued way of “giving back” to community members who had referred participants to us.
Designate a point person to coordinate dissemination outreach. Once the initial plan was outlined, we reached out to CBOs to explore their interest in hosting presentations. The study coordinator served as a point person for this process. Although the whole research team was active in dissemination, having a point person allowed community members to communicate with us easily, facilitated our addressing their concerns, and helped us tailor presentations to audiences. This role required experience working in the community, an ability to convey findings accurately without jargon, and readiness to answer questions about study aims, history, challenges, and community feedback.
Draw on established relationships. Relationships are at the heart of CBPR (1), and the dialogues initiated through interactive presentations created opportunities to strengthen our existing relationships with CBOs and community members by demonstrating that their support — through participation, referrals, or guidance — had resulted in important research findings. Ideally, the research team should have established relationships with key community gatekeepers before the dissemination phase. Several team members had long histories of engagement with the local community, and these relationships were often deepened through CAB meetings and during data collection. For example, while obtaining medical records to track patients’ engagement in care, the study coordinator developed a stronger working relationship with a local physician who treated many of the patients. During the dissemination phase, this same physician recommended our presentation as content for a continuing education series and then helped to facilitate an engaging discussion.
Conduct “pre-meetings” with gatekeepers. As the first step in scheduling presentations, the study coordinator initiated conversations with CBO staff members to explain our findings, to explore their possible relevance for staff members or clients, and to offer to conduct a presentation and co-facilitate a discussion. The study coordinator and CBO staff members also planned logistics and strategized together about how to ensure a good fit between content and attendees. This process began by exploring the interests and expertise of likely attendees and identifying which findings fit those interests so that slides could be tailored. The conversation also addressed how to attract attendees who would benefit from the presentation and contribute to discussions. We found that CBO staff members who had close relationships with clients were often able to identify and invite individuals or groups who cared about the research topic and about fostering a productive dialogue.
Work with community members to select findings for presentation. To select the overall content, we shared a broad set of findings with our CAB and asked what they thought would be of interest to community members. We then tailored this general set of findings to various audiences, such as community forums, client meetings, staff meetings, or continuing education trainings. We found that attendees at large community forums (eg, regional planning meetings where consumers and CBO representatives make recommendations on HIV-related services and funding) tended to be research-oriented and interested in precise descriptions of methods and policy implications. In contrast, meetings of CBO staff members or clients emphasized how findings could be pragmatically applied to services (eg, a one-page handout with tips for addressing clients’ mistrust). Continuing education trainings (eg, with nurses and physicians) allowed more time than other venues, enabling us to cover findings in more depth and facilitate more nuanced discussions. Continuing education attendees are regularly exposed to recent research findings at other trainings but rarely have opportunities to discuss the findings with the researchers who have conducted the studies.
Make presentations interactive. To foster dialogue, we included community members and CBO staff members as co-facilitators and reserved as much time for discussion as for the presentation. Whenever possible, CBO staff members helped to facilitate discussions, which led to rich dialogues combining our familiarity with the findings with their experience in the community. A project interviewer presented the methods, which strengthened rapport with attendees because he had also established relationships with CBO staff members during the study’s recruitment phase.
Share a personal story illustrating how the issue has affected your life. Although our research team includes several black staff members, the principal investigator and the on-site co-investigator, who often led presentations, are white. During presentations they were sometimes asked why they were doing research with black communities. In exploring these questions with the CAB, it became clear that there were concerns that nonblack researchers might be motivated by factors other than the well-being of the community, such as professional opportunism or financial gain. The team understood how such concerns could arise from both the historical and ongoing marginalization of black communities in research, health care, and other contexts. To build rapport and trust, the CAB suggested that the primary presenter address mistrust at the beginning of the presentation by telling a story that conveyed why this area of research mattered personally. When we implemented this advice, the effect in the room was palpable, establishing a feeling of personal connection between the attendees and the speaker. The story was of an experience of HIV stigma that occurred when the principal investigator, as a teenager, had requested an HIV test from her doctor, who responded in a judgmental manner, saying “We don’t have patients like that here.” She shared with the audience how that experience deepened her commitment to understanding and addressing HIV stigma through research. In addition to clarifying the speaker’s motives, sharing this story helped to humanize the research topic.
Cultivate a receptive attitude toward criticism. Part of seeking community feedback on research involves receiving criticism on the study’s methods, interpretation of findings, or overall approach. At such times, it may be tempting to respond defensively, for example by suggesting that the concerns are somehow less applicable to the study or researchers in question. However, we sought to adopt a receptive stance toward such comments by responding in a respectful, nonconfrontational manner. Defensive responses may undermine trust and exacerbate community concerns about researchers by dismissing the validity and relevance of their comments. We found that it was important to inquire further, seek to better understand the concerns, respond to them, learn from them, and revise our research strategies accordingly. We also came to appreciate how such comments led to deeper and more authentic conversations about issues implicit in doing research with black communities in the United States. They demonstrated community members’ investment in the research and their community — an investment that is crucial to respect and nourish in CBPR. By the end of the project, many community members confirmed that our efforts to listen to, and learn from, criticism was among the most important factors that made the study successful from a community perspective.
Follow up with one-on-one meetings. After presentations, some attendees reached out to us to discuss parallels between their work as service providers and our findings. Setting up face-to-face meetings or conference calls helped to solidify new relationships and enabled us to engage in much more detailed and realistic explorations of how community partners’ work shed light on the findings, implications of the findings for their programs, and possible collaborations.
Recognize the potential value of research findings for service providers. Following presentations at community forums, some CBO leaders wanted to discuss how the findings related to their programs. One CBO used our preliminary data for a grant proposal, allowing for timely use of research findings (a key aim of CBPR). In another case, we presented data (from another study) to a local funder that was considering cutting funding for a community partners’ program — a program that our data suggested was yielding strong positive outcomes. For CBOs that develop new interventions, data can also suggest which aspects of their program may contribute most to improving outcomes. For example, staff members from one CBO discussed how their intervention, although developed intuitively through community input, was based on principles similar to those shown in our findings. To make findings most useful for providers, be prepared to develop brief reports or conduct tailored analyses.
Demonstrate that suggestions are integrated into further research or programs. In follow-up meetings, attendees and our CAB also told us that one of the most important aspects of the process was seeing that their input was implemented. Integrating feedback from presentations and follow-up conversations demonstrated to community members that the discussions were not merely academic exercises but represented mutual learning opportunities with positive effects on clients, programs, and further research.
We developed a dissemination process for CBPR involving a series of interactive community presentations held at local CBOs. This process was intended to deepen our understanding of our study findings, support near-term implementation by providers, strengthen relationships with community partners, and elicit ideas for culturally relevant interventions. Although researchers frequently emphasize the importance of these types of aims (4–7), few report on implementation of strategies to achieve them. Through post-presentation research team debriefings and systematic review of notes from presentations, we identified a set of concrete strategies that researchers can use to engage communities in two-way conversations about research findings. These include creating a flexible dissemination plan, tailoring presentations to various community groups, establishing a point person to serve as a community liaison, and continuing dialogue with CBOs and attendees after presentations. Keys to developing trust during dissemination included engaging community members at every step, reserving ample time for discussion during presentations, building rapport by sharing personal experiences, being receptive to and learning from criticism, and implementing community members’ input.
We found these strategies beneficial, but our findings are limited because they reflect the dissemination process of only one project. Further research is needed to determine whether the strategies can consistently foster community trust, cultural tailoring of findings, or near-term implementation by community providers. Future research could also compare different strategies. For example, as an alternative to delivering interactive presentations at CBOs, community members could be invited to day-long forums (26), which have the potential advantage of increasing one-on-one dialogue between community members and researchers. However, briefer interactive presentations may be better for reaching a wide array of community members through integration into standing meetings at CBOs, continuing education trainings, and other existing settings.
In light of growing concern that communities do not always receive the benefits of new findings (27), researchers are encouraged to design studies with community dissemination in mind (28,29). Our study illustrates how community dissemination plans that include strategies for dialogue may yield benefits beyond those limited to one-way dissemination. These strategies can be incorporated into dissemination plans and research proposals, which should specify the overall approach to be used (eg, interactive presentations) and how the approach will be implemented (eg, with a point person for community relations). Plans should also be flexible to enable responsiveness to community input and reflect the concerns of the communities being studied. For example, with populations that are historically mistrustful of research, it is important to articulate how trust has been developed or will be fostered in meaningful ways.
Conducting dissemination as a dialogue with community members involves an investment of time and resources, but it can lead to understanding of findings that is well-grounded in community perspectives and their implications for existing and new community-based services. In addition, this type of dissemination can strengthen community–academic partnerships, which builds 1) community trust in research and 2) researchers’ understanding of community concerns. New research findings may be of interest to community members, particularly if they are able to use them in proposals and programs. Given the labor-intensiveness of community dissemination, funders who support CBPR should be prepared to designate adequate resources so that community members may genuinely take an active role in all phases of research and use data for practical purposes, such as improving their programs or influencing public policy at the community level (28). For example, the National Cancer Institute developed supplemental grants for dissemination that may serve as a model for targeted dissemination; and our experience suggests it is valuable for community dissemination to be incorporated into primary funding mechanisms to encourage “designing for dissemination” (29). Similarly, academic settings should reward efforts to facilitate community dialogue on research findings, which may yield benefits not only to individual studies but also to the overall reputation of research in diverse communities.
This research was funded by National Institute of Minority Health and Health Disparities R01MD003964 and R01MD006058 (L.M.B., principal investigator). Support for manuscript preparation was also provided by P30 AI060354 (B.D. Walker, PI). We also gratefully acknowledge the members of APLA’s Research Community Advisory Board, whose valued input was crucial to facilitating an effective and engaging community dissemination process, as well as the Harvard University Center for AIDS Research Community Advisory Board, which provided essential input on lessons learned.
Corresponding Author: Bryce McDavitt, PhD, AIDS Project Los Angeles, 611 South Kingsley Dr, Los Angeles, CA 90005. Telephone: 213-201-1447. Email: [email protected] .
Author Affiliations: Laura M. Bogart, Boston Children’s Hospital, Boston, Massachusetts, Harvard Medical School, Boston, Massachusetts, RAND Corporation, Santa Monica, California; Matt G. Mutchler, AIDS Project Los Angeles, Los Angeles, California, California State University, Dominguez Hills, Carson, California; Glenn J. Wagner, Harold D. Green, Jr, RAND Corporation, Santa Monica, California; Sean Jamar Lawrence, Kelsey A. Nogg, AIDS Project Los Angeles, Los Angeles, California; Kieta D. Mutepfa, UCLA CARE Center, Los Angeles, California. Dr McDavitt is also affiliated with University of Southern California, Los Angeles, California and Pacifica Graduate Institute, Carpinteria, California.
- Griffin JP, Yancey E, Armstrong-Mensah E. Building partnerships in community-based participatory research. In: Blumenthal DS, Smith S, Braithwaite RL, DiClemente RJ, editors. Community-based participatory health research: issues, methods, and translation to practice. New York (NY): Springer Publishing Company; 2013. p. 19–34.
- Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman JR. Critical issues in developing and following community-based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco (CA): Jossey-Bass; 2003. p. 53–76.
- Chen PG, Diaz N, Lucas G, Rosenthal MS. Dissemination of results in community-based participatory research. Am J Prev Med 2010;39(4):372–8. CrossRef external icon PubMed external icon
- Hacker K. Community-based participatory research. Thousand Oaks (CA): Sage Publications; 2013.
- Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco (CA): Jossey-Bass; 2005. Chapter 1, Introduction to methods for CBPR for health; p. 3–26.
- Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA; The Cochrane Effective Practice and Organization of Care Review Group. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ 1998;317(7156):465–8. CrossRef external icon PubMed external icon
- Bogart LM, Uyeda K. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol 2009;28(4):391–3. CrossRef external icon PubMed external icon
- Resnicow K, Davis R, Zhang N, Tolsma D, Alexander G, Wiese C, et al. Tailoring a fruit and vegetable intervention on ethnic identity: results of a randomized study. Health Psychol 2009;28(4):394–403. CrossRef external icon PubMed external icon
- Rhodes SD, Hergenrather KC, Montaño J, Remnitz IM, Arceo R, Bloom FR, et al. Using community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Educ Prev 2006;18(5):375–89. CrossRef external icon PubMed external icon
- Bogart LM, Bird ST, Walt LC, Delahanty DL, Figler JL. Association of stereotypes about physicians to health care satisfaction, help-seeking behavior, and adherence to treatment. Soc Sci Med 2004;58(6):1049–58. CrossRef external icon PubMed external icon
- Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. J Acquir Immune Defic Syndr Hum Retrovirol 1998;18(4):341–8. CrossRef external icon PubMed external icon
- Bogart LM, Wagner G, Galvan FH, Banks D. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among African American men with HIV. J Acquir Immune Defic Syndr 2010;53(5):648–55. PubMed external icon
- Bogart LM, Galvan FH, Wagner GJ, Klein DJ. Longitudinal association of HIV conspiracy beliefs with sexual risk among black males living with HIV. AIDS Behav 2011;15(6):1180–6. CrossRef external icon PubMed external icon
- Mathes T, Pieper D, Antoine SL, Eikermann M. Adherence-enhancing interventions for highly active antiretroviral therapy in HIV-infected patients — a systematic review. HIV Med 2013;14(10):583–95. CrossRef external icon PubMed external icon
- Simoni JM, Amico KR, Smith L, Nelson K. Antiretroviral adherence interventions: translating research findings to the real world clinic. Curr HIV/AIDS Rep 2010;7(1):44–51. CrossRef external icon PubMed external icon
- Amico KR, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. J Acquir Immune Defic Syndr 2006;41(3):285–97. CrossRef external icon PubMed external icon
- Canadian Health Services Research Foundation. Communication notes: developing a dissemination plan. Ottowa (ON): CHSRF; 2004.
- Crosswaite C, Curtice L. Disseminating research results: the challenge of bridging the gap between health research and health action. Health Promot Int 1994;9(4):289–96. CrossRef external icon
- Fernández-Peña JR, Moore L, Goldstein E, Decarlo P, Grinstead O, Hunt C, et al. Making sure research is used: community-generated recommendations for disseminating research. Prog Community Health Partnersh 2008;2(2):171–6. CrossRef external icon PubMed external icon
- Cashman SB, Allen AJ, Corburn J, Israel BA, Montano J, Rhodes SD, et al. Analyzing and interpreting data with communities. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health: from process to outcomes. Hoboken (NJ): John Wiley & Sons; 2008. p. 285–302.
- Christopher S, Watts V, McCormick AKHG, Young S. Building and maintaining trust in a community-based participatory research partnership. Am J Public Health 2008;98(8):1398–406. CrossRef external icon PubMed external icon
- Earl CE, Penney PJ. The significance of trust in the research consent process with African Americans. West J Nurs Res 2001;23(7):753–62. CrossRef external icon PubMed external icon
- Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans’ views on research and the Tuskegee Syphilis Study. Soc Sci Med 2001;52(5):797–808. CrossRef external icon PubMed external icon
- Hoover MA, Green HD Jr, Bogart LM, Wagner GJ, Mutchler MG, Galvan FH, et al. Do people know I’m poz?: factors associated with knowledge of serostatus among HIV-positive African Americans’ social network members. AIDS Behav 2015. PubMed external icon
- Wallerstein N, Duran B, Minkler M, Foley K. Developing and maintaining partnerships with communities. In: Israel BA, Eng E, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. Hoboken (NJ): Jossey-Bass; 2005. p. 31–51.
- Lopez EDS, Parker E, Edgren K, Brakefield-Caldwell W. Disseminating research findings back to partnering communities: lessons learned from a community-based participatory research approach. Metrop Univ J 2005;16:57–76.
- Green LW, Ottoson JM, García C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health 2009;30(1):151–74. CrossRef external icon PubMed external icon
- National Cancer Institute. Designing for dissemination: conference summary report. Washington (DC): National Cancer Institute; 2002.
- Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health 2013;103(9):1693–9. CrossRef external icon PubMed external icon
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
- Apply now Enquire now
Study at UniSA
Accounting and Finance Business Management and HRM Marketing Property Tourism, Sports and Events
Architecture Communication Contemporary Art Creative Industries Design Film, Television and Visual Effects Journalism Urban and Regional Planning
Biomedical Science Health Science Human Movement, Sport, Clinical Exercise Physiology Laboratory Medicine Medical Radiation Science Nursing or Midwifery Nutrition and Food Sciences Occupational Therapy Pharmacy Physiotherapy Podiatry Speech Pathology
- Law & Criminal Justice
Aboriginal and Australian Studies Arts Human Services Languages Psychology Social Work
Aviation Construction Management Defence Engineering Environmental Science Information Technology Mathematics Science
- Teaching & Education
- What can I study
- Entry pathways
- Find an education agent
- Sponsorships
- Living in Adelaide
- UniSA Online
- Scholarships
- Postgraduate study
- Research degrees
- Executive Education
- Regional students
- Aboriginal students
- Discover our research Partner with us
- Research projects
- How to apply
- Check your eligibility
- Research scholarships
- Concentrations
- Cooperative Research Centres
- Research studies & volunteers
- Research experts
- Industry & collaboration
- Mawson Lakes
- Mount Gambier
- Psychology Clinic
- Health Clinics
- Disability Hub
- Wirringka Student Services
- Museums and galleries
- Industry & partnerships
- Enterprise Hub
About UniSA
- Our history
- Vice Chancellor
- Achievements
- Mission, values, vision
- Strategic action plan
- Staff directory
- UniSA Allied Health & Human Performance
- UniSA Business
- UniSA Clinical & Health Sciences
- UniSA Creative
- UniSA Education Futures
- UniSA Justice & Society
- Working at UniSA
- Publications
- Aboriginal engagement
- Login Staff Students Alumni
- Research Integrity and Ethics
- Responsible research practice
Dissemination of research
Dissemination of research findings is an important part of the research process, passing on the benefits to other researchers, professional practitioners and the wider community. Research activities supported by public funding are rarely considered complete until the results have been made widely available.
There are many ways of disseminating research findings. Formal publication of the results of research most commonly takes place in refereed academic journals or books, but this is not always the case. This section of the Framework applies to all forms of dissemination of research findings, refereed and non-refereed, in any medium of communication, including conferences, public performance and public exhibition.
The University of South Australia is committed to promoting an environment of honesty, integrity, accuracy and responsibility in the dissemination of research findings by:
- ensuring that all parties to the research are made aware of the nature and scope of confidentiality agreements;
- protecting the intellectual property rights of the institution, the researcher, research trainees and sponsors of the research, as appropriate;
- ensuring in sponsored research arrangements that the sponsors of research understand the importance of publication in research and do not delay publication beyond the time needed;
- protecting intellectual property and other relevant interests;
- ensuring that researchers are aware of contractual arrangements that restrict, delay or limit publication;
- assisting researchers in effective communication through the mass media by the provision of advice, guidance, information resources and training opportunities;
- supporting communication of research findings to the wider public by, for example, assistance through the University's policy, Public statements by members of University staff ; and
- making every effort when reporting research results for publicity purposes to acknowledge partner institutions and sponsors involved in collaborative research.
The University seeks to promote the dissemination of research findings in a manner consistent with the requirements of the Australian Code for the Responsible Conduct of Research , which states in R23 that researchers should “Disseminate research findings responsibly, accurately and broadly. Where necessary, take action to correct the record in a timely manner.”
This Section should also be read in conjunction with the following University policies: Authorship (RES-12) ; Intellectual Property: Ownership and Management Policy (RES-22) ; Public statements by members of University staff (C-5) .
Directly related UniSA policies, procedures and forms
- Authorship Policy RES-12
- Public statements by members of University staff
- University Activities - Intellectual Property: Ownership and Commercialisation Guidelines
- direction-signage-arrows-signs Also in this section plus-thin minus-thin Research Integrity and Ethics Responsible research practice minus-thin plus-thin General principles of responsible research Data integrity and management Managing conflicts of interest Authorship Plagiarism Dissemination of research Use of funding Peer review Collaborative research across institutions Relationships Supervision of trainees Research ethics minus-thin plus-thin Human ethics Animal ethics Biosafety and permits Policies, procedures, codes and legislation Contact us minus-thin plus-thin Research Integrity Advisors Concerns and complaints Research Ethics and Safety Innovation Awards
Australian students
Phone: +61 8 8302 2376 Enquiry: unisa.edu.au/enquiry
International students
Phone: +61 8 9627 4854 Enquiry: unisa.edu.au/enquiry

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 06 November 2024
Science communication will benefit from research integrity standards
You have full access to this article via your institution.
An anti-vaccination protester in New York City. Researchers are aiming to improve public trust in science by discussing uncertainty in their communications. Credit: Michael Nigro/Pacific Press/LightRocket/Getty
“Twenty seconds, professor, and no long words.” This is what a BBC producer once told Ian Fells, a chemical engineer at Newcastle University, UK, shortly before Fells was due to appear on a live broadcast. It was more than 30 years ago, at a time when few researchers were trained in how to condense science into sound bites, while staying true to the accuracy of their message.
Today, that challenge could be even bigger. The smartphone makes every researcher a potential writer, audio producer or broadcaster. Although many scientists have taken to communicating directly with the public , others are afraid to do so, not least because social-media platforms offer few guardrails or protections against disinformation. Another reason for their hesitancy is that principles that are fundamental to research — such as the scientific process, uncertainty around the results and the context — are difficult to fit into fast and short content formats.

Science must protect thinking time in a world of instant communication
Rhys Morgan, head of research policy, governance and integrity at the University of Cambridge, UK, has a fairly radical — or at least unusual — proposal. In a report published last month by the League of European Research Universities (LERU), a network of 24 institutions, Morgan proposes that public-facing science-communication work should adhere to the same research-integrity principles that are used for scholarly publications, and suggests that universities should support scientists who do so (see go.nature.com/4hxw4ag ). In journal articles, researchers describe the methods used to obtain their findings and whether, for example, animals or artificial-intelligence tools were used in experiments; they explain how a finding fits in with the current knowledge in a field and declare conflicts of interest.
The idea deserves more attention from universities, companies and campaigning organizations — all of which are now much more involved in science communication than at any time in the past. It might not work in all contexts and there will be challenges to its implementation, but the concept should be discussed more widely.
There’s a view in the world of professional communication — for example, in companies that provide media training — that people prefer certainty to uncertainty. There are also studies that support this idea, not least the work of Daniel Ellsberg (published before he became famous for revealing a classified US study on the Vietnam war). The problem with emphasizing certainty as the default option when communicating science to a wider audience is that this is not how researchers discuss their findings in scholarly journals. In such instances, data are often communicated as a range, with levels of confidence in the results. Most researchers are careful not to overstate a finding, or use language that could be misinterpreted to mean certainty. Communicating results that sound certain when they are provisional could also harm a researcher’s reputation. Public trust in science, already under strain in many countries, could be further reduced ( C. Dries et al. Public Underst. Sci. 33 , 777–794; 2024 ).

Bring PhD assessment into the twenty-first century
The LERU report doesn’t go into how Morgan’s proposals could be implemented. But there are important implications, for corporate, government and university media offices. Many press officers work closely with scientists to ensure science is communicated accurately both on social media and in conventional mass media. They go out of their way to find researchers who have knowledge about and passion for what they do. However, at some institutions, staff members have fewer resources to communicate research results, compared with in the past, according to a 2022 report on the changing role of university press officers by science-communication consultant Helen Jamison for the Science Media Centre in London (see go.nature.com/3ccqxba ). This is in part because many senior leaders in universities regard press-office communication as mainly about boosting their institute’s profile and reputation. Morgan and Jamison’s reports suggest that scientists need to be supported better by their institutions and recognized for their efforts in research communications, too.
Communicating uncertainty is often difficult, but there are tools and research available to those willing to try. ‘How to Communicate Uncertainty’, a 2020 report by researcher Dora-Olivia Vicol at the University of Oxford, UK, summarizes some of the literature nicely and provides helpful suggestions, such as how to effectively discuss a range of values and what the impact on audiences is when different words are used to describe uncertainty (see go.nature.com/3ufox9j ). It was published by a consortium of fact-checking organizations: Africa Check in Johannesburg, Chequeado in Buenos Aires and London-based Full Fact. This shows that the ideas proposed by Morgan were already on the radar in this communications sector.
Science communication can do more to embrace uncertainty. It’s up to everyone who talks about research to consider describing both the process and the outcomes of the work — even in a 20-second sound bite with no long words.
Nature 635 , 8 (2024)
doi: https://doi.org/10.1038/d41586-024-03586-w
Reprints and permissions
Related Articles

- Research management
- Scientific community

Grass-roots pressure grows to boost support for breastfeeding scientists
Career Feature 08 NOV 24

‘Anyone engaging in scientific practice shouldn’t be excluded’: The United Kingdom’s only Black chemistry professor, on diversity
Career Q&A 06 NOV 24

I had to let a student go and I feel as though I failed them — how do I do better next time?
Career Feature 04 NOV 24
Distributed peer review: how Ukraine has reaped the benefits and minimized the risks
Correspondence 05 NOV 24

Is there a ‘Goldilocks zone’ for paper length?
Nature Index 05 NOV 24

What Trump’s election win could mean for AI, climate and health
News 08 NOV 24

Will South Africa become first country to accept controversial form of human genome editing?
News 07 NOV 24
Southeast University Future Technology Institute Recruitment Notice
Professor openings in mechanical engineering, control science and engineering, and integrating emerging interdisciplinary majors
Nanjing, Jiangsu (CN)
Southeast University
Open Faculty Positions at the State Key Laboratory of Brain Cognition & Brain-inspired Intelligence
The laboratory focuses on understanding the mechanisms of brain intelligence and developing the theory and techniques of brain-inspired intelligence.
Shanghai, China
CAS Center for Excellence in Brain Science and Intelligence Technology (CEBSIT)
Faculty Positions in School of Engineering, Westlake University
The School of Engineering (SOE) at Westlake University is seeking to fill multiple tenured or tenure-track faculty positions in all ranks.
Hangzhou, Zhejiang, China
Westlake University
2025 International Young Scholars Forum of International School of Medicine, Zhejiang University
Researchers in the fields of life sciences, healthcare, or the intersection of medicine, industry, and information technology.
Yiwu, Zhejiang, China
International School of Medicine, Zhejiang University
Tenure-track Assistant Professor - Inflammation, Metabolism, or Therapeutic Targeting
Washington D.C. (US)
The George Washington University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Digital Health
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Sexual Health
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
National Academies President on How to Use Generative AI Responsibly in Scientific Research
- 1 Editor in Chief, JAMA
- 2 Associate Editor, JAMA
- Editorial Guidance on Reporting Use of AI in Research and Scholarly Publication Annette Flanagin, RN, MA; Romain Pirracchio, MD, MPH, PhD; Rohan Khera, MD, MS; Michael Berkwits, MD, MSCE; Yulin Hswen, ScD, MPH; Kirsten Bibbins-Domingo, PhD, MD, MAS JAMA
- Original Investigation Excess Death Rates for Republican and Democratic Voters in Florida and Ohio During the COVID-19 Pandemic Jacob Wallace, PhD; Paul Goldsmith-Pinkham, PhD; Jason L. Schwartz, PhD JAMA Internal Medicine
This conversation is part of a series of interviews in which JAMA Network editors and expert guests explore issues surrounding the rapidly evolving intersection of artificial intelligence (AI) and medicine.
AI tools are transforming scientific research and publishing, but they are also raising important questions about how science will be conducted responsibly in the AI era.
Marcia McNutt, PhD
The National Academy of Sciences (NAS) is one of the leading organizations working on ways to uphold scientific integrity while leveraging AI’s potential to advance knowledge. In an editorial published in the Proceedings of the National Academy of Sciences this May, NAS President Marcia McNutt, PhD, and more than 20 coauthors from academia, industry, and government presented key principles for conducting research that uses generative AI. The authors cautioned that although AI will speed scientific discoveries, its tools and processes—particularly generative AI—challenge some of the “core norms and values in the conduct of science, including accountability, transparency, replicability, and human responsibility.”
McNutt and her coauthors also called on the scientific community to build oversight bodies that can respond to the use of AI in scientific research. To that end, they proposed that the National Academies of Sciences, Engineering, and Medicine create a Strategic Council on the Responsible Use of Artificial Intelligence in Science.
JAMA and JAMA Network Editor in Chief Kirsten Bibbins-Domingo, PhD, MD, MAS, recently spoke with McNutt, a geophysicist and a former editor in chief of the journal Science , about the opportunities for using generative AI to aid scientific research—and the principles that should guide researchers as they employ it. McNutt’s first piece of guidance? “Disclose, disclose, disclose.”
This interview has been edited for clarity and length.
Dr Bibbins-Domingo: Could you explain what the National Academy of Sciences is? What role does it have when we think about new innovations that challenge and provide opportunities in our field?
Dr McNutt: The National Academy of Sciences has been around for more than 160 years. It was founded by Abraham Lincoln during the darkest days of the Civil War, and he wanted the scientists on his side. He wanted to be able to consult with the nation’s top scientists whenever there was an opportunity for evidence, whether it’s basic science, engineering, or medicine, to better inform public decisions. The National Academy of Sciences is now joined by the National Academy of Engineering and the National Academy of Medicine. And we have served as an apolitical, unbiased reservoir of information to help the nation make better decisions about disease and new technologies.
Dr Bibbins-Domingo: Certainly, the need to have science inform policy decisions in various sectors is still present today. What has the National Academy of Sciences’ role been in thinking about the new generative AI tools and what they might mean for science?
Dr McNutt: The National Academy of Sciences activated its members, employees, and committees very early on. There have been bespoke applications of AI that have been around for decades. My background is in marine science, and we have used AI on underwater vehicles for decades. There is no way to effectively communicate through saltwater with complex engineering devices, whether they be autonomous observatories or autonomous underwater vehicles. AI was the one way to get the most out of these technologies at a time when a direct connection to the human brain was not possible. I think the concerns that I have heard voiced most often have to do with large language models or generative AI, because this is AI moving into a new realm. Whenever we put AI on underwater vehicles or in spacecraft or anything else where it’s difficult to connect to the human brain, we could always test whether the AI was doing exactly what we wanted it to do. One of the first topics that came up at the National Academy in terms of concerns about generative AI had to do with the norms of science. As scientists, we value work that is reproducible. You can put the same query into a generative AI model and get 2 different answers. Reproducibility is just not part of the generative AI way of working. The other thing we really respect in terms of a science norm is attribution. If you are using work that was previously done, you have to cite who did it and what they said. For generative AI, this stuff comes out and you have no idea where it came from. When references are provided, sometimes they’re made up. A third norm is transparency. In scientific publishing, we value complete transparency of how we got to an answer. What did we use? What was our thinking? What were our preconceived assumptions? We know nothing of that with generative AI. So we held a retreat to which we invited some of the AI leaders from industry, academia, and government to explore what we can do to ensure that the norms of science are promoted and are supported in this brave new world. We started with the most important thing: human responsibility. We must hold generative AI users responsible for how they use it and what they conclude. If they haven’t taken the time to double check what’s coming out of generative AI, that’s on them. We have pushed for AI developers to make it easier for users to understand what the preconceived starting points for any solution were. We have made it imperative that researchers who use generative AI cite that they have, show exactly what in their research was the result of generative AI, and explain what they did to verify the results. I think that is one of the biggest issues we’ve dealt with. But another concern that I’ve had is that I don’t see the public sufficiently involved. We have a number of other cases of new technologies that were very promising but got off to a bad start because of the lack of public understanding, particularly of the safeguards, the appropriate uses, and the misuses. One good example is GMOs [genetically modified organisms]. Look at how quickly the public, particularly in Europe, became very, very suspicious of GMOs. With these genetically modified organisms, I think so many people saw only industry engaging in it, so they felt that the only applications of genetically modified organisms were for corporate profit. The lesson I take from that is we have to be very concerned that academia is being priced out of AI research. The size of research grants is simply insufficient to support new model development at universities. And I fear that if only industry is promoting and developing AI, we will quickly lose public trust.
Dr Bibbins-Domingo: When you have a new technology that is clearly so powerful and has so much potential to further the science for publishing and a variety of other modes of communication, it’s exciting. The only thing you can do in the end is say that humans ultimately still bear the responsibility. By the time we published an editorial in JAMA earlier this year that said humans still sign the author integrity form, it was amazing that ChatGPT had already been indexed as an author on several publications. And it speaks to how fast we start to say, “Well, yeah. This would be fine. If I had this tool, it could actually be an author.” In the end, ultimately, we must hold ourselves accountable as individual researchers and as a collective scientific and medical community. That’s one of the most important things. I think we as scientists—and I’m a clinician as well—are learning how to use the tools effectively and responsibly. We worry, “Can I trust that figure in that paper?” And we figure out the rules. But if the public can’t trust in that same way, that is another level of loss that is really important for our collective communities.
Dr McNutt: I agree completely, and we’ve already struggled in recent years with trust in science. It all started with climate change, with people feeling that the efforts they would need to take to counter climate change were going to be so distasteful in terms of their quality of life that they didn’t want to do it. I never felt that human health would fall victim to the same lack of public trust. Because it seems to me there is no special interest group as there was for tobacco or as there was for oil. There’s no special interest group that is going to take pride out of trying to discount science because it’s in their personal financial benefit. But when it came to human health, I honestly couldn’t believe that we were dealing with misinformation and people putting out statements that were actually harmful to people’s health. And I think it was JAMA [ Internal Medicine ] that published that paper that showed the difference between the death rate because of [the difference in COVID-19] vaccine uptake of people who were registered in the 2 different political parties. And it actually made a life-or-death difference as to whether you were sucked in by that misinformation.
Dr Bibbins-Domingo: It’s an interesting time to think about technologies that can enable us to have information that we can put on many different types of platforms, that we can create and disseminate from original research articles, that might reach a lay audience, that might reach audiences in different languages so much more easily. That is one of the things that these tools do extraordinarily well. That is such a boon for helping to deliver high-quality information to so many more people, especially as it relates to science, as it relates to their health. At the same time, it is concerning if more people become mistrustful because images can be manipulated and even we can’t quite figure out how to attribute the right citation to that piece of information or we can’t reproduce it. How do we engage the public and how do we engage other scientists in the conversations about what we need to do to use these tools responsibly in a way that the scientific community and the broader public can trust?
Dr McNutt: I’m not sure I know of any scientist right now who is not engaging with AI. As you say, it is a remarkable tool. There’s not a day that goes by that I don’t use AI. But I am very careful about how I use it, and I am very suspicious anytime I get something back that looks odd. One great example of that was I had a whole bunch of people I had to introduce once at a National Academy meeting. So I asked ChatGPT, “Can you just give me a 4-sentence summary of why this person is so terrific or whatever?” All 4 of them were winners of the National Medal of Science, according to the AI, but actually none of them were. AI had inferred, based on their distinguished background, that of course they must be recipients of the National Medal of Science, even though that was demonstrably wrong by going to the National Medal of Science webpage and looking at who has received it.
Dr Bibbins-Domingo: That’s a great example of both the widespread use and why we still all have to have that healthy skepticism and understand these tools better. You’ve been a journal editor and you now run an organization that is convening and helping to provide the thought leadership on what we should be doing. Is it enough for our journals to say, “You as an author are responsible as you always have been for the integrity of the work that appears on these pages.” That when the different major media outlets pick up this work, they can say, “Well, we trust that it’s in these pages and we trust that the authors have said this. Therefore, the public should trust that these findings are important.” Is that enough?
Dr McNutt: I’m just not sure that will be enough because it’s sort of like saying to people, “Well, we have this tool. You don’t understand it. We don’t really understand it either. But we’re going to use it, and so you should trust it.” That’s not going to get us anywhere. I would say that first of all, disclose, disclose, disclose. It’s so important in every paper to say at every step of the way what tools were involved and what you learned. Disclose, disclose, disclose how you checked the results. You can only build trust. This is part of science. It’s not until findings have been reproduced, ideally with similar results, and also extended—that the results were so strong that we could actually make predictions in other systems that were proven to be correct, which is a completely independent way of verifying results. And I think this is the same approach we’re going to have to take with generative AI.
Dr Bibbins-Domingo: In the end, the enduring pieces to the scientific enterprise really are about the transparency, the rigorous reporting, and the reproducibility for other scientists. And that’s why we don’t have confidence in 1 article or 1 experiment but trust the entire scientific process.
Dr McNutt: It’s basically independent verification. There was so much basic science that went into the creation of chips, for example, that we have in our cell phones and our computers and everything else. No one distrusts that science because the devices actually work. They work as they were designed and intended based on the physics that was learned through that research. We’re going to have to get to that stage with generative AI, too, where the proof is in the results. But that’s going to take disclosure and testing at every step of the way. I try to focus mostly on impacts of AI and science. But as you well know, AI is going to be pervasive. Some of the applications will be testable, others may be a little more difficult. For example, everyone’s concerned about how AI will be used in image recognition. I heard this fascinating story on the news the other day about a grocery store that, instead of putting a paper price on a shelf for what these items cost, is thinking of dynamic pricing. And so, if there’s a run on toilet paper because people think another disease is coming, the store can jack up the price of toilet paper to try to discourage that from happening. I thought to myself, “Can you imagine dynamic pricing being combined with AI so that what happens is as you walk up to the shelf, the AI determines, ‘Oh, she can afford to pay more. Let’s up the price by another dollar.’ And someone else walks up and it says, ‘Oh, this person looks like they’re on hard times. We’re going to lower the price for them.’” These applications are not pipe dreams. They could actually happen.
Dr Bibbins-Domingo: It sounds like there’s going to be a lot of need for more convenings of the National Academy of Sciences and scientists to figure this out. I think your point of having the scientific community actively engaged in this so that it is not just with the large corporations is a key piece. I would really underscore that as a medical community, as a scientific community, that even if the actual workings of these technologies are not always obvious, understanding what they mean for our fields is important. Ultimately, the principles by which we self-govern require that all of us know enough to engage so that it isn’t something that is just left to the large corporate interests, which are clearly there.
Dr McNutt: I recently put together a presentation with 65 slides about activities on AI that the Academy has underway, ranging from how AI can be used to help with very, very difficult mathematical proofs to how AI can be used for better natural hazard prediction like hurricanes and floods and things like that. We’re also looking at how AI could exacerbate climate change through the dramatic power requirements that are needed, and AI in social sciences and life sciences research. Right before generative AI came on the scene, a lot of scientists were recognizing we had very, very large datasets in which it was very, very difficult to find patterns. Now we can do that.
Dr Bibbins-Domingo: Clearly, what’s ahead of us is exciting and requires that all of us engage. It’s great to see that it’s a priority of the National Academy of Sciences.
Dr McNutt: At the last NAS annual meeting, we had a panel on AI. And one of the questions from the audience was, “How will we ever trust AI since we don’t understand, even the engineers don’t understand, exactly how it works, how it spits out its answers?” And one of the panelists said, “We don’t understand that for the human brain either. And yet, we still have mechanisms for building trust in our fellow humans.” And I think that’s going to have to be where we start for building trust in AI.
Published Online: November 8, 2024. doi:10.1001/jama.2024.14025
Conflict of Interest Disclosures: Dr McNutt reported that the NAS publishes 3 journals: PNAS , PNAS Nexus , and Issues in Science and Technology .
See More About
Bibbins-Domingo K , Hswen Y. National Academies President on How to Use Generative AI Responsibly in Scientific Research. JAMA. Published online November 08, 2024. doi:10.1001/jama.2024.14025
Manage citations:
© 2024
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

IMAGES
COMMENTS
4. Manage the timeline and resources. Time constraints are an inevitable part of research dissemination. Deadlines for publications can be months apart, conferences may only happen once a year, etc. Any avenue used to disseminate the research must be carefully planned around to avoid missed opportunities.
Dissemination of research is still largely ruled by the written or spoken word. However, there are many ways to introduce visual elements that can act as attractive means to help your audience understand and interpret your research. Disseminate findings through art or multimedia interpretations.
Most applied health research funding agencies expect and demand some commitment or effort on the part of grant holders to disseminate the findings of their research. However, there does appear to be a lack of clarity between funding agencies as to what represents dissemination [ 9 ].
The researcher interview guide was designed to understand researchers' perspectives on communicating and disseminating research findings to participants; explore past experiences, if any, of researchers with communication and dissemination of research findings to study participants; document any approaches researchers may have used or intend ...
Why are dissemination and implementation research as well as diffusion research important? ... Inadequate communication and dissemination can be a barrier to timely and effective implementation of research findings. Therefore, dissemination research is another means for increasing the probability of moving research discoveries to sustained ...
Let's explore some strategies to help keep your dissemination plan on track. Why do I need a research dissemination plan? A dissemination plan is the key to sharing your research findings with the right audiences, including the public, professionals, and policymakers. Making your research more accessible and relatable maximizes its value and ...
Box 1 Summary of research dissemination. What—Dissemination of health and medical research entails communicating the findings of research to stakeholders in ways that can facilitate understanding and use.. Why—Any positive, inconclusive or negative research findings should be disseminated to maximise the social value of the research and to accurately inform medical policies and practices.
Understand how and where your audience looks for/receives information. Gain an insight into what motivates your audience and the barriers they may face. Remember to feedback study findings to participants, such as patients and clinicians; they may wish to also participate in the dissemination of the research and can provide a powerful voice.
Rule 3: Encourage participation. In the age of open research, don't just broadcast. Invite and engage others to foster participa-tion and collaboration with research audiences. Scholarship is a collective endeavour, and so we should not expect its dissemination to be unidirectional, especially not in the digital age.
How we communicate research is changing because of new (especially digital) possibilities. This article sets out 10 easy steps researchers can take to disseminate their work in novel and engaging ...
Dissemination of research results is an important aspect of the research process because it ensures that the benefits of the study are passed on to others and that it is put to good use. A research's proper dissemination is however supposed to draw the attention of governments or stakeholders to the research's outcomes, giving a social ...
Introduction: Translating research findings into practice requires understanding how to meet communication and dissemination needs and preferences of intended audiences including past research participants (PSPs) who want, but seldom receive, information on research findings during or after participating in research studies. Most researchers want to let others, including PSP, know about their ...
Why is Dissemination so Difficult? Disconnect between research and practice slows adoption of promising findings Perverse incentives: peer-reviewed publications lead to promotions and tenure; research raises more questions Lack of access to expert communications resources Need to use different languages with different audiences
Abstract. Dissemination and communication of research should be considered as an integral part of any research project. Both help in increasing the visibility of research outputs, public engagement in science and innovation, and confidence of society in research. Effective dissemination and communication are vital to ensure that the conducted ...
Disseminating the Findings of your Research Study. It is very important to find appropriate ways to disseminate the findings of your research - projects that sit on office or library shelves and are seldom or never read represent a tragic loss to the profession. A key dimension of research dissemination is to be actively involved with ...
Background: Addressing deficiencies in the dissemination and transfer of research-based knowledge into routine clinical practice is high on the policy agenda both in the UK and internationally.However, there is lack of clarity between funding agencies as to what represents dissemination. Moreover, the expectations and guidance provided to researchers vary from one agency to another.
Step 1: Check-in with your JHU media office if you think your findings are newsworthy. Media attention is one of the most efficient ways to broadly disseminate findings, and the communications team can help. Also check-in with the journal's media office to see if they have interest in promoting the findings. Step 2: If the communications team ...
Dissemination is "the intentional, active process of identifying target audiences and tailoring communication strategies to increase awareness and understanding of evidence and motivate its use in policy, practice, and individual choice" (PCORI ). 1 Simply put, dissemination is about getting research results to the people who can benefit from those findings.
10 TIPS FOR IMPROVING RESEARCH VISIBILITY Expand your co-authorship base. In addition to the usual benefit of bringing new expertise and ideas to the paper, co-authoring with a diverse group of colleagues helps to disseminate research findings more widely. 4, 5 To impact changes in policy and/or practice, potential policy makers should be engaged early on, preferably right from the conception ...
Dissemination research is defined as the scientific study of the targeted distribution of information and intervention materials to a specific public health, clinical practice, or policy audience. ... This attention to end-user perspectives is intended to help ensure the research findings will have clear utility to communities, practices, and ...
Dissemination and communication of research should be considered as an integral part of any research project. ... was an essential component of the project in order to achieve the purpose of fostering policy change based on research findings. Here we provide our experience and make some recommendations based on our learning. A strong use of ...
Sharing research findings with community members is a vital component of community-based participatory research (CBPR) for several reasons (1,2). First, community members deserve access to the knowledge they have made possible through participation or other forms of engagement in a study (3). Second, community dissemination creates ...
Dissemination of research findings is an important part of the research process, passing on the benefits to other researchers, professional practitioners and the wider community. Research activities supported by public funding are rarely considered complete until the results have been made widely available. There are many ways of disseminating ...
In journal articles, researchers describe the methods used to obtain their findings and whether, for example, animals or artificial-intelligence tools were used in experiments; they explain how a ...
Dr Bibbins-Domingo: It's an interesting time to think about technologies that can enable us to have information that we can put on many different types of platforms, that we can create and disseminate from original research articles, that might reach a lay audience, that might reach audiences in different languages so much more easily. That ...