This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013; 36:S67-S74 https://doi.org/10.2337/dc13-S067
Bilous R, Donnelly R. Handbook of diabetes, 4th edn. Chichester: Wiley-Blackwell; 2010
Boore J, Cook N, Shepherd A. Essentials of anatomy and physiology for nursing practice.London: Sage; 2018
Brackney DE. Enhanced self-monitoring blood glucose in non-insulin-requiring type 2 diabetes: a qualitative study in primary care. J Clin Nurs. 2018; 27:(9–10)2120-2131 https://doi.org/10.1111/jocn.14369
Buchanan TA, Xiang A, Kjos SL, Watanabe R. What is gestational diabetes?. Diabetes Care. 2007; 30:S105-S111 https://doi.org/10.2337/dc07-s201
Accu-check Inform II system. 2018. https://tinyurl.com/y3ersrht (accessed 27 March 2018)
Dean L, McEntyre J. The genetic landscape of diabetes.Bethseda (MD): National Centre for Biotechnology Information; 2004
Essentials of nursing practice, 2nd edn. In: Delves-Yates C (ed). London: Sage; 2018a
Delves-Yates C Essential clinical skills for nurses: step by step, 2nd edn. (ed). London: Sage; 2018b
The Royal Marsden manual of clinical nursing procedures, Professional edition. 9th edn. In: Dougherty L, Lister S (eds). Chichester: Wiley Blackwell; 2015
Holt P. Blood glucose monitoring in diabetes. Nurs Stand. 2014; 28:(27)52-58 https://doi.org/10.7748/ns2014.03.28.27.52.e650
Holt TA, Kumar S. ABC of diabetes, 7th edn. Chichester: Wiley Blackwell/BMJ Books; 2015
Hortensius J, Slingerland RJ, Kleefstra N Self-monitoring of blood glucose: the use of the first or the second drop of blood. Diabetes Care. 2011; 34:(3)556-560 https://doi.org/10.2337/dc10-1694
International Diabetes Federation. Diabetes atlas. 2017. http://diabetesatlas.org/resources/2017-atlas.html (accessed 27 March 2019)
Joint Formulary Committee. Hypoglycaemia. Treatment of hypoglycaemia. Treatment summary. 2019. https://bnf.nice.org.uk/treatment-summary/hypoglycaemia.html (accessed 27 March 2019)
Mabrey ME, Setji TL. Patient self management of diabetes care in the inpatient setting: pro. J Diabetes Sci Technol. 2015; 9:(5)1152-1154 https://doi.org/10.1177/1932296815590827
Marieb EN, Hoehn K. Human anatomy and physiology, 10th edn. Harlow: Pearson Education; 2015
Medicines and Healthcare products Regulatory Agency. Blood glucose meters: point of care testing—advice for healthcare professionals. 2013. https://tinyurl.com/y6ro3aoj (accessed 27 March 2019)
Maughan R. Carbohydrate metabolism. Surgery. 2009; 27:(1)6-10 https://doi.org/10.1016/j.mpsur.2008.12.002
National Institute for Health and Care Excellence. Type 1 diabetes in adults: diagnosis and management. NICE guideline NG17. 2016a. https://www.nice.org.uk/guidance/ng17 (accessed 27 March 2019)
National Institute for Health and Care Excellence. Diabetes (type 1 and type 2) in children and young people: diagnosis and management. NICE guideline NG18. 2016b. https://www.nice.org.uk/guidance/ng18 (accessed 27 March 2019)
National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. NICE guideline NG28. 2017a. https://www.nice.org.uk/guidance/ng28 (accessed 27 March 2019)
National Institute for Health and Care Excellence. FreeStyle Libre for glucose monitoring. 2017b. https://www.nice.org.uk/advice/mib110 (accessed 27 March 2019)
Patton K, Thibodeau G. Anatomy and physiology, 9th edn. St Louis (MO): Mosby Elsevier; 2015
Sanders LM. Carbohydrate: digestion, absorption and metabolism. In: Caballero B, Finglas PM, Toldra F (eds). Oxford: Academic Press; 2016
Shah AD, Rushakoff RJ. Patient self-management of diabetes care in the inpatient setting: Con. J Diabetes Sci Technol. 2015; 9:(5)1155-1157 https://doi.org/10.1177/1932296815586581
Shaji S, Rajendran D, Kumpatla S, Viswanathan V. Evaluation of diabetes self-care with self-monitoring of blood glucose among type 2 diabetic patients and its impact on HbA1c. International Journal of Diabetes in Developing Countries. 2013; 33:(3)181-182 https://doi.org/10.1007/s13410-013-0118-2
Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013; 12:(1) https://doi.org/10.1186/2251-6581-12-14
Training Research and Education for Nurses in Diabetes (Trend) UK. Blood glucose guidelines. Consensus document. 2017. https://tinyurl.com/y8zq4lmw (accessed 27 March 2019)
Blood glucose monitoring in diabetes: rationale and procedure
Charlotte Gordon
Lecturer, Adult Nursing, Department of Nursing Midwifery and Health, Northumbria University, Newcastle upon Tyne, and Member, Royal College of Nursing National Steering Group Committee for Diabetes
View articles · Email Charlotte
Diabetes mellitus is a condition that results in elevated blood glucose levels. Continued elevation can contribute to progressive micro- and macrovascular complications, leading to renal, nerve and ocular damage, representing a significant contributor to patient morbidity and mortality. The measurement of blood glucose provides information on the effectiveness of blood glucose metabolism and guides interventions to achieve optimal glucose control within the body. All nurses should be familiar with the importance of blood glucose monitoring and the procedure to carry out testing safely and effectively. Appropriate and timely monitoring of blood glucose will allow for the successful management of blood glucose that is out of the target range. This will ensure ongoing patient safety during episodes of acute illness or effective management of diabetes mellitus in the longer term, minimising future diabetic-related health complications.
Diabetes mellitus is a condition that results in elevated blood glucose levels (hyperglycaemia). Continued elevation can contribute to progressive micro- and macrovascular complications leading to renal, nerve and ocular damage, representing a significant contributor to morbidity and mortality ( Bilous and Donnelly, 2010 ). Currently there are more than 3 million adults (aged 18–99) diagnosed with the condition in the UK, representing a population prevalence of 5.9%; 1 in 17 adults has diabetes mellitus ( International Diabetes Federation (IDF), 2017 ).
Type 1 diabetes mellitus represents approximately 10% of cases. The origin of the condition is autoimmune in nature, arising from the complete destruction of insulin-secreting beta cells within the pancreas. Type 1 diabetes results in an absolute absence of insulin and therefore blood glucose levels continue to rise because glucose cannot enter the body's cells to be metabolised and produce energy; excess glucose cannot be stored as glycogen. These individuals require insulin injections every day.
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
19.2 Blood Glucose Monitoring
Blood glucose monitoring is performed on patients with diabetes mellitus and other conditions that cause elevated blood sugar levels. Diabetes mellitus is a common medical condition that affects the body’s ability to produce insulin in the pancreas and use insulin at the cellular level. There are two types of diabetes mellitus, type 1 and type 2. Type 1 diabetes mellitus is an autoimmune disease that damages the beta cells of the pancreas so they do not produce insulin; thus, synthetic insulin must be administered by injection or infusion. It typically begins in childhood or adolescence. Type 2 diabetes mellitus accounts for approximately 95 percent of all cases and is highly correlated with obesity and inactivity. During type 2 diabetes, the cells of the body become resistant to the effects of insulin, and the pancreas increases its production of insulin. However, over time, the pancreas may no longer be able to produce insulin. In many cases, type 2 diabetes can be managed by moderate weight loss, regular physical activity, and a healthy diet. However, if blood glucose levels cannot be controlled with healthy lifestyle choices, oral diabetic medication is prescribed and eventually, the administration of insulin may be required. [1] Prediabetes is a medical condition where blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Approximately one in three American adults have prediabetes. Gestational diabetes is a type of diabetes that occurs during pregnancy in women who did not have diabetes before they were pregnant.
Diabetic patients require frequent blood glucose monitoring to administer customized medication therapy to prevent long-term complications from occurring. Hospitalized patients who do not have diabetes may also require frequent blood glucose monitoring due to elevations that can occur as a result of the stress of hospitalization, surgical procedures, and side effects of medications. Additionally, patients receiving enteral feedings typically have their blood glucose monitored every six hours. Health care providers prescribe the frequency of blood glucose monitoring; testing is typically performed before meals and at bedtime. For some patients, a standardized sliding-scale insulin protocol may be prescribed with instructions on the medication administration record (MAR) for administration of insulin based on their blood glucose results. [2] , [3] See Table 19.2 for an example of a sliding-scale insulin protocol.
Table 19.2 Sample Sliding-Scale Insulin Protocol
Instructions: Check patient’s blood sugar before meals, at bedtime, and as needed for symptoms of hypoglycemia or hyperglycemia. Use the following table to administer insulin lispro PRN.
| Less than 70 | Hold all insulin and initiate hypoglycemia protocol. |
|---|---|
| 70-150 | 0 units |
| 151-174 | 2 units |
| 175-199 | 4 units |
| 200-224 | 6 units |
| 225-249 | 8 units |
| 250-274 | 10 units |
| 275-299 | 12 units |
| Greater than 300 | Administer 14 units and call the provider. |
Hypoglycemia
When caring for patients with diabetes mellitus and monitoring their blood glucose readings, it is important to continually monitor for signs of hypoglycemia. Hypoglycemia is defined as blood sugar readings less than 70 and signs and symptoms such as the following:
- Feeling nervous or anxious
- Sweating, chills, and clamminess
- Irritability or impatience
- Fast heartbeat
- Feeling light-headed or dizzy
- Color draining from the skin (pallor)
- Feeling sleepy
- Feeling weak or having no energy
- Blurred/impaired vision
- Tingling or numbness in the lips, tongue, or cheeks
- Coordination problems or clumsiness
- Nightmares or crying out during sleep
- Seizures [4]
A low blood sugar level triggers the release of epinephrine (adrenaline), the “fight-or-flight” hormone. Epinephrine causes the symptoms of hypoglycemia such as a rapid heartbeat, sweating, and anxiety. If a patient’s blood sugar level continues to drop, the brain has impaired functioning. This may lead to seizures and a coma. [5]
If a nurse suspects hypoglycemia is occurring, a blood sugar reading should be obtained, and appropriate actions taken. Most agencies have a hypoglycemia protocol based on the “15-15 Rule.” The 15-15 Rule is to provide 15 grams of carbohydrate and recheck the blood glucose after 15 minutes. If the reading is still below 70 mg/dL, another serving of 15 grams of carbohydrate should be provided and the process continued until the blood sugar is above 70 mg/dL. Fifteen grams of carbohydrate includes options like 4 ounces of juice or regular soda, hard candy, or glucose tablets. If a patient is experiencing severe hypoglycemia and cannot swallow, a glucagon injection or intravenous administration of dextrose may be required. [6]
Hyperglycemia
Hyperglycemia is defined as elevated blood glucose and often causes signs and symptoms such as frequent urination and increased thirst. Hyperglycemia occurs when the patient’s body does not produce enough insulin or cannot use the insulin properly at the cellular level. There are many potential causes of hyperglycemia, such as not receiving enough medication to effectively control blood glucose, eating more than planned, exercising less than planned, or increased stress from an illness, surgery, hospitalization, or other life events.
If a patient’s blood glucose is greater than 240 mg/dL, their urine is typically checked for ketones. Ketones indicate a condition called ketoacidosis may be occurring. Ketoacidosis occurs in patients whose pancreas is no longer creating insulin, so fats are broken down for energy and waste products called ketones are produced. If the kidneys cannot effectively eliminate ketones in the urine, they build up in the blood and cause ketoacidosis. Ketoacidosis is a life-threatening condition that requires immediate notification of the provider for treatment. Symptoms of ketoacidosis include fruity-smelling breath, nausea, vomiting, very dry mouth, and shortness of breath. Treatment of ketoacidosis often requires the administration of intravenous insulin while the patient is closely monitored in a critical care inpatient unit. [7]
For more information about diabetes mellitus, measuring blood sugar levels, and diabetic medications, visit the “ Endocrine ” chapter in Open RN Nursing Pharmacology .
Glucometer Use
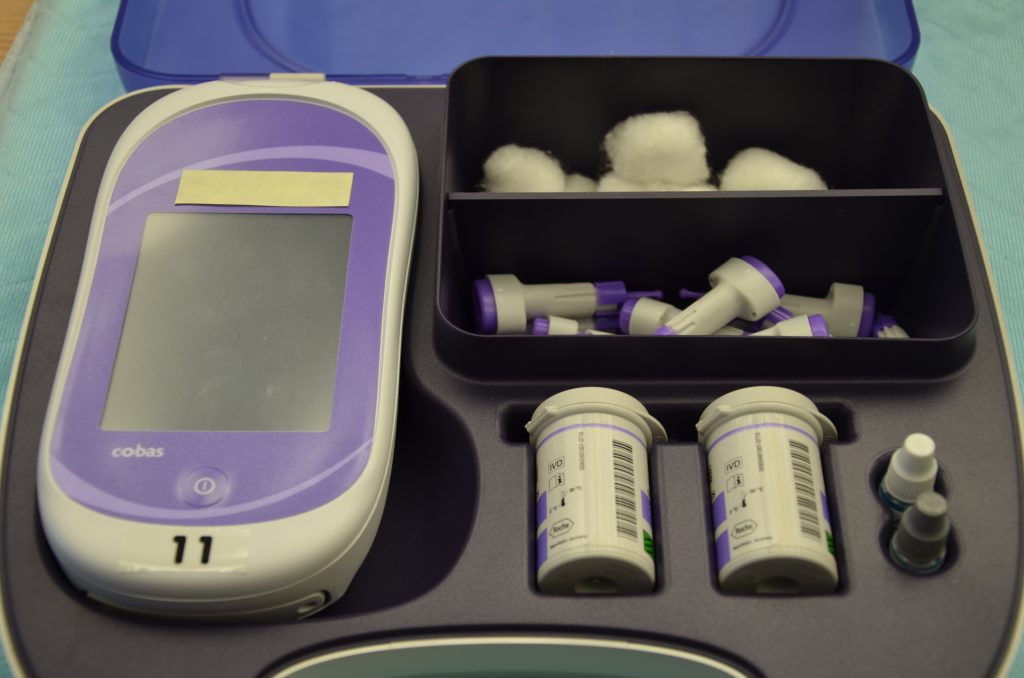
It is typically the responsibility of a nurse to perform bedside blood glucose readings, but in some agencies, this procedure may be delegated to trained nursing assistants or medical assistants. See Figure 19.1 [8] for an image of a standard bedside glucometer kit that contains a glucometer, lancets, reagent strips, and calibration drops. Prior to performing a blood glucose test, read the manufacturer’s instructions and agency policy because they may vary across devices and sites. Ensure the glucometer has been calibrated per agency policy. [9]
Before beginning the procedure, determine if there are any conditions present that could affect the reading. For example, is the patient fasting? Has the patient already begun eating? Is the patient demonstrating any symptoms of hypoglycemia or hyperglycemia? Keep your patient safe by applying your knowledge of diabetes, the medication being administered, and the uniqueness of the patient to make appropriate clinical judgments regarding the procedure and associated medication administration. [10]
See the “ Checklist for Blood Glucose Monitoring ” for details regarding the procedure. It is often important to keep the patient’s hand warm and in a dependent position to promote vasodilation and obtain a good blood sample. If necessary, warm compresses can be applied for 10 minutes prior to the procedure to promote vasodilation. Follow the manufacturer’s instructions to prepare the glucometer for measurement. After applying clean gloves, clean the patient’s skin with an alcohol wipe for 30 seconds, allow the site to dry, and then puncture the skin using the lancet. See Figure 19.2 [11] for an image of performing a skin puncture using a lancet.

If needed, gently squeeze above the site to obtain a large drop of blood. Do not milk or massage the finger because it may introduce excess tissue fluid and hemolyze the specimen. Wipe away the first drop of blood and use the second drop for the blood sample. Follow agency policy and manufacturer instructions regarding placement of the drop of blood for absorption on the reagent strip. See Figure 19.3 [12] for an image of a nurse absorbing the patient’s drop of blood on the reagent strip. Timeliness is essential in gathering an appropriate specimen before clotting occurs or the glucometer times out.

Cleanse the glucometer and document the blood glucose results according to agency policy. Report any concerns about patient symptoms or blood sugar results according to agency policy.
Life Span Considerations
Blood glucose samples should be taken from the heel of newborns and infants up to the age of six months. When obtaining a sample from the heel, the sample is taken from the medial or lateral plantar surface.
View a supplementary YouTube video on Obtaining a Bedside Blood Glucose [13]
- This work is a derivative of Nursing Pharmacology by Open RN licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Donihi, A. C., DiNardo, M. M., DeVita, M. A., & Korytkowski, M. T. (2006). Use of a standardized protocol to decrease medication errors and adverse events related to sliding scale insulin. Quality & Safety in Health Care, 15 (2), 89–91. https://doi.org/10.1136/qshc.2005.014381 ↵
- American Diabetes Association. (n.d.). Hypoglycemia (Low blood sugar) . https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hypoglycemia (Low blood sugar). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hyperglycemia (High blood glucose). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hyperglycemia ↵
- “DSC_0718.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- “DSC_1130.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- “DSC_1141.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 . Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- RegisteredNurseRN. (2015, August 12). How to prick fingertips with a lancet device for checking a blood sugar | Nursing skills [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/JPJ4l7QZ9eM ↵
Standardized instructions for administration of adjustable insulin dosages based on a patient’s premeal blood glucose readings.
A blood glucose reading less than 70 associated with symptoms such as irritability, shakiness, hunger, weakness, or confusion.
A rule included in an agency’s hypoglycemia protocols that includes providing 15 grams of carbohydrate, then repeating the blood glucose reading in 15 minutes, and then repeating as needed until the patient’s blood glucose reading is above 70.
Elevated blood glucose reading with associated signs and symptoms such as frequent urination and increased thirst.
A life-threatening complication of hyperglycemia that can occur in patients with Type 1 Diabetes Mellitus that is associated with symptoms such as fruity-smelling breath, nausea, vomiting, severe thirst, and shortness of breath.
Nursing Skills - 2e Copyright © 2023 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Effects of Guided Reflection on Diabetes Self-Care: A Randomized Controlled Trial
Affiliations.
- 1 School of Nursing, Rhode Island College, Providence, Rhode Island.
- 2 Department of Adult Nursing, University of Massachusetts Dartmouth, North Dartmouth, Massachusetts.
- 3 Diabetes Care Solutions LLC, Greenville, Rhode Island.
- 4 Assumption College, Worchester, Massachusetts.
- PMID: 30501480
- DOI: 10.1177/0145721718816632
The purpose of this study was to evaluate the effects of guided reflection on self-care behaviors, confidence scores, and diabetes knowledge among adults with diabetes. A randomized controlled trial with a pre/posttest design was used to generate data from a convenience sample of 62 adults with diabetes recruited from a single site. After viewing a 30-minute video on how to manage diabetes, participants were randomized to a control group (CG) (usual care) or an intervention group (IG). The IG further engaged in a reflection educational session. For 8 weeks, the IG isolated diabetes-related events weekly, critically analyzed them using Gibbs's reflective questions, and recorded their analysis in a journal. They also shared their perspective relative to using the journal in an audiotaped interview. Main measures included baseline and 8-week clinical outcomes (self-care maintenance, monitoring, management, and confidence scores and diabetes knowledge scores) and intervention acceptability. Compared to the CG, the IG had no statistically significant difference in self-care measures over time, although scores trended in the anticipated direction. Importantly, both groups had statistically significant improvement in self-care scores. Furthermore, there was statistically significant improvement in diabetes knowledge among IG participants. Informatively, IG critically analyzed 147 diabetes-related events concentrating on blood glucose, diet, exercise, monitoring, medication, sleep pattern, and health care visits. Participants found the guided reflection activity highly acceptable. Combined educational and reflection interventions are effective approaches for improving self-care outcomes and diabetes knowledge among adults with diabetes. Research concentrating on purposeful patient reflection is warranted in a larger sample paying careful attention to study limitations.
PubMed Disclaimer
Similar articles
- Effects of guided imagery on outcomes of pain, functional status, and self-efficacy in persons diagnosed with fibromyalgia. Menzies V, Taylor AG, Bourguignon C. Menzies V, et al. J Altern Complement Med. 2006 Jan-Feb;12(1):23-30. doi: 10.1089/acm.2006.12.23. J Altern Complement Med. 2006. PMID: 16494565 Free PMC article. Clinical Trial.
- Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. Hill-Briggs F, Lazo M, Peyrot M, Doswell A, Chang YT, Hill MN, Levine D, Wang NY, Brancati FL. Hill-Briggs F, et al. J Gen Intern Med. 2011 Sep;26(9):972-8. doi: 10.1007/s11606-011-1689-6. Epub 2011 Mar 29. J Gen Intern Med. 2011. PMID: 21445680 Free PMC article. Clinical Trial.
- Randomized clinical trial of an integrated self-care intervention for persons with heart failure and diabetes: quality of life and physical functioning outcomes. Dunbar SB, Reilly CM, Gary R, Higgins MK, Culler S, Butts B, Butler J. Dunbar SB, et al. J Card Fail. 2015 Sep;21(9):719-29. doi: 10.1016/j.cardfail.2015.05.012. Epub 2015 May 29. J Card Fail. 2015. PMID: 26028261 Free PMC article. Clinical Trial.
- Behavioral and Pharmacotherapy Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: An Updated Systematic Review for the U.S. Preventive Services Task Force [Internet]. LeBlanc EL, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. LeBlanc EL, et al. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Sep. Report No.: 18-05239-EF-1. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Sep. Report No.: 18-05239-EF-1. PMID: 30354042 Free Books & Documents. Review.
- Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force [Internet]. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Patnode CD, et al. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017 Jul. Report No.: 15-05222-EF-1. Rockville (MD): Agency for Healthcare Research and Quality (US); 2017 Jul. Report No.: 15-05222-EF-1. PMID: 29364620 Free Books & Documents. Review.
- A Self-Report Measure of Diabetes Self-Management for Type 1 and Type 2 Diabetes: The Diabetes Self-Management Questionnaire-Revised (DSMQ-R) - Clinimetric Evidence From Five Studies. Schmitt A, Kulzer B, Ehrmann D, Haak T, Hermanns N. Schmitt A, et al. Front Clin Diabetes Healthc. 2022 Jan 13;2:823046. doi: 10.3389/fcdhc.2021.823046. eCollection 2021. Front Clin Diabetes Healthc. 2022. PMID: 36994332 Free PMC article.
- SGLT2 inhibitor versus carbohydrate-restricted isocaloric diet: reprogramming substrate oxidation in type 2 diabetes. Igarashi H, Uchino H, Kanaguchi M, Hisanaga K, Sato G, Yoshikawa F, Furuta M, Washizawa N, Usui S, Miyagi M, Hirose T. Igarashi H, et al. Diabetol Metab Syndr. 2023 Feb 19;15(1):25. doi: 10.1186/s13098-023-00990-6. Diabetol Metab Syndr. 2023. PMID: 36804863 Free PMC article.
- Undertaking Healthy Nutrition Behaviors by Patients with Type 1 Diabetes as an Important Element of Self-Care. Sińska BI, Dłużniak-Gołaska K, Jaworski M, Panczyk M, Duda-Zalewska A, Traczyk I, Religioni U, Kucharska A. Sińska BI, et al. Int J Environ Res Public Health. 2022 Oct 13;19(20):13173. doi: 10.3390/ijerph192013173. Int J Environ Res Public Health. 2022. PMID: 36293753 Free PMC article.
- [Development and Validation of the Self-Care for Aspiration Pneumonia Prevention Scale in the Community Dwelling Elderly with Risk of Dysphasia]. Yang EY, Lee SY. Yang EY, et al. J Korean Acad Nurs. 2020 Jun;50(3):474-486. doi: 10.4040/jkan.20041. J Korean Acad Nurs. 2020. PMID: 32632079 Korean.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Genetic Alliance
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Reflection on Achieving Blood Glucose Monitoring Objectives
Learning objective:
To understand the importance of blood glucose monitoring in diabetes management and to learn effective techniques for accurate monitoring
Reflection: Did you achieve the set objectives within the allocated time frame? Briefly describe. What would you do differently next time in similar situations?
Introduction
The learning objective of comprehending the significance of blood glucose monitoring in diabetes management and mastering accurate monitoring techniques is essential for effective diabetes care. This reflection essay delves into whether the set objectives were achieved within the allocated time frame, offering insights into the experience and potential improvements for similar situations.
Objective Achievement and Time Frame
The set objectives were indeed achieved within the allocated time frame. Through engaging instructional sessions, practical demonstrations, and hands-on practice, I gained a profound understanding of the importance of blood glucose monitoring in diabetes management. Furthermore, I acquired effective techniques to ensure accurate monitoring, including proper device usage, calibration, and interpretation of results.
Experience and Learning Highlights
The journey of attaining these objectives was enlightening. The interactive nature of the learning sessions fostered an engaging environment, allowing me to grasp the nuances of blood glucose fluctuations and their impact on diabetes management. The hands-on practice provided a tangible experience, enabling me to translate theoretical knowledge into real-world applications.
Identification of Improvements
While the objectives were successfully met, there are aspects I would consider refining for future similar situations: Enhanced Practice Opportunities: Incorporating more hands-on practice sessions could further solidify the skills acquired. Additional practice time would help build confidence in using monitoring devices and interpreting results accurately.
Real-Life Case Studies: Integrating real-life case studies and scenarios into the learning process would offer a comprehensive understanding of the challenges individuals with diabetes face in managing their blood glucose levels. This approach would foster empathy and reinforce the importance of accurate monitoring.
Collaborative Learning: Encouraging peer discussions and group activities could promote shared insights and diverse perspectives on blood glucose monitoring. Collaborative learning facilitates a dynamic exchange of experiences and strategies for effective diabetes management.
Incorporating Technological Tools: As technology continues to evolve , incorporating digital tools and apps that simulate blood glucose monitoring scenarios could enhance the learning experience. Simulated scenarios allow for safe exploration of various monitoring situations and decision-making processes.
Conclusion: Continuous Improvement in Learning
The journey to achieving the blood glucose monitoring objectives was a rewarding experience. The interactive and hands-on approach facilitated an in-depth understanding of diabetes management and accurate monitoring techniques. While the objectives were met, the potential for improvement lies in refining practice opportunities , integrating real-life scenarios, fostering collaborative learning, and utilizing technological tools. By continuously enhancing the learning process, we ensure that individuals equipped with these skills are better prepared to contribute to effective diabetes management and provide comprehensive care to those in need.
Approximate price: $ 22
Recent Posts
- Exploring Self-Concept Development in Children: Insights from the Video Assignment
- Empowering Families: A Comparative Analysis of Family Psychoeducation Models
- Nurturing Well-being: Examining the Program Components of Planet Health
- Navigating Vulnerability and Setting Goals for Meaningful Connections
- Navigating the Night: Strategies for College Students to Improve Sleep Hygiene
Recent Comments
Calculate the price of your order.
- Free title page and bibliography
- Unlimited revisions
- Plagiarism-free guarantee
- Money-back guarantee
- 24/7 Customer support
- Tutor’s samples
- Part-by-part delivery
- Overnight delivery
- Attractive discounts
- Expert Proofreading
- 275 words per page
- 12 pt Arial/Times New Roman
- Double line spacing
- Any citation style (APA, MLA, Chicago/Turabian, Harvard)
Unique Features
As a renowned provider of the best writing services, we have selected unique features which we offer to our customers as their guarantees that will make your user experience stress-free.
Money-Back Guarantee
Unlike other companies, our money-back guarantee ensures the safety of our customers' money. For whatever reason, the customer may request a refund; our support team assesses the ground on which the refund is requested and processes it instantly. However, our customers are lucky as they have the least chances to experience this as we are always prepared to serve you with the best.
Zero-Plagiarism Guarantee
Plagiarism is the worst academic offense that is highly punishable by all educational institutions. It's for this reason that Peachy Tutors does not condone any plagiarism. We use advanced plagiarism detection software that ensures there are no chances of similarity on your papers.
Free-Revision Policy
Sometimes your professor may be a little bit stubborn and needs some changes made on your paper, or you might need some customization done. All at your service, we will work on your revision till you are satisfied with the quality of work. All for Free!
Privacy And Confidentiality
We take our client's confidentiality as our highest priority; thus, we never share our client's information with third parties. Our company uses the standard encryption technology to store data and only uses trusted payment gateways.
High Quality Papers
Anytime you order your paper with us, be assured of the paper quality. Our tutors are highly skilled in researching and writing quality content that is relevant to the paper instructions and presented professionally. This makes us the best in the industry as our tutors can handle any type of paper despite its complexity.
WhatsApp Us
- Print this reflection
- Email a link to this reflection
REFLECTIVE LEARNING FORM Evidence for revalidation and appraisals

| Mrs Anu Mathew | Nurse (Associate, Community, District, Practice, School, Staff, Surgical, etc) |
| Safe Use of Insulin in Hospital | Core |
| 21st May 2023 | 45 mins |
| CDEP is a competency-based online diabetes learning tool that supports all levels of health and social care workers confirm their diabetes knowledge relevant to their role. CDEP is based on the UK diabetes competency frameworks which structure the level of diabetes skills required by health and social care staff to promote safer patient care, improved outcomes and reduce the financial burden of diabetes. |
| Be aware of the function, use and side effects of insulin therapy in people living with diabetes in hospital. Be aware of the common types of insulin and their use in the management of diabetes. Be aware of the common insulin delivery devices and be able to safely utilise them. Be able to appropriately monitor glucose levels in people with insulin-treated diabetes. Be able to competently inject insulin. Have an understanding of the right timing of insulin doses in common hospital scenarios. Be aware of how to use a variable rate intravenous insulin infusion (VRIII) safely. Be aware of common insulin errors and how they can be prevented. |
| On a scale of 1 to 5: |
| How would you rate your overall level in diabetes patient care since completing this topic? 5 / 5 How would you rate your overall with managing patients with diabetes since completing this topic?5 / 5 How would you rate your overall familiarity with in relation to diabetes practice since completing this topic?5 / 5 |
| What have you learnt from undertaking this topic? The safe use of insulin in diabetic patient and management of hypoglycemia and hyperglycemia. Types of insulin Monitoring of blood glucose levels Safe administration of insulin using correct 10 step injection process Health education for patient regarding safe use of insulin pens and monitoring of blood glucose levels How may you adapt your practice as a result of this topic? The topic helped me to enhance my knowledge in safe use of Insulin in Hospital. It will help me to prioritize and identify deteriorating patients and the need for blood glucose monitoring thus avoiding hypoglycemia and hyperglycemia in patients. I make sure the monitoring of blood glucose does timely according to the administration and mechanism of action of different types of insulin. I will be able to notify patients to DSN for effective interventions and appropriate management of diabetics to avoid any complications. Were there any additional learning needs identified as a result of this topicNO How is this CPD relevant to your profession's code of conduct and / or practice standards? Please provide further detailsPrioritise people by making sure that any treatment under my responsibility is delivered without undue delay to avoid any complications in diabetic patients Practice effectively- work in partnership with medical team and DSN to make sure the diabetic patients are cared effectively. Preserve safety- ask for help from suitably qualified and experienced professional as needed Provide professionalism and trust- Encourage to build a trusting relationship with patient and maintain a professional attitude at all times in managing and educating regarding diabetic mellitus. |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Utilization of Blood Glucose Data in Patient Education
Yaa kumah-crystal.
Vanderbilt University Medical Center, Department of Pediatrics, Monroe Carell Jr. Children’s Hospital at Vanderbilt, 2200 Children’s Way DOT Room 11142-C, Nashville, TN 37232-9170
Shelagh Mulvaney
Vanderbilt University Medical Center, School of Nursing, Department of Pediatrics, & Department of Biomedical Informatics, 461 21st Avenue South, Nashville, TN 37240
Many studies have tested clinical and behavioral approaches for improving glycemic control in people with diabetes. We review research to identify how blood glucose (BG) values have been used in patient-focused clinical research and interventions. We sought to describe the frequency that BG values have been the focus of patient education research and to characterize the different methods to integrate BG into an intervention, the approaches implemented to support patient education and behavior change, and the nature of communication about BG values. Thirty-four eligible studies were identified that included patient education using BG values. Information regarding the study and intervention characteristics include: 1) Characteristics of the study sample, 2) How BG values were obtained, 3) Use of a graphical interface for BG values, 4) Use of a BG log, 5) BG interpretation and regimen adjustments, 6) Recommended actions to patient, 7) Modality of intervention, and 8) Intervention communication schedule. The review demonstrated that new BG technologies provide outstanding opportunities for greater access to BG data, and for patient support and intervention. However, it also indicated a need to improve and expand support for people with diabetes in their daily use of BG values to maintain and improve glycemic control. In order to make the most sustainable impact on behavior, generalizable skills such as problem solving need to be integrated into BG education.
Introduction: Background
Self-monitoring of blood glucose (BG) levels is critical to the daily self-management for people with diabetes. In people with type 1 diabetes (T1D) the Diabetes Control and Complications Trial (DCCT) demonstrated that intensive insulin regimens and BG control corresponded with better glycemic control and resulted in a significant decrease in the macro- and microvascular complications of diabetes [ 1 , 2 ]. A similar finding was noted in the type 2 diabetes (T2D) population with the United Kingdom Prospective Diabetes Study (UKPDS), which also demonstrated evidence of improved outcomes when participants engaged in a more intensive management course compared to the standard therapy [ 3 ]. While A1C was the major outcome variable in the DCCT and UKPDS, it is a person’s level of adherence and blood glucose control that largely determines A1C [ 4 ]. A critical component of adherence is BG monitoring to guide insulin and behavioral adjustments on a day-to-day and meal-to-meal basis [ 5 ].
Patient education around interpretation of BG values initially occurs shortly after diagnosis with diabetes when patients are taught target BG ranges, and how to adjust carbohydrate and insulin intake to maintain euglycemia. In T1D and insulin treated T2D, patients are given an algorithm by which to interpret a BG value, determine their dosing based on their meal intake, and to use a sliding insulin scale to compensate for varying BG values. This is the fundamental concept behind how a closed loop BG monitoring and insulin-dispensing device would operate [ 6 ]. However, when a person with diabetes is solely responsible for these assessments, and the adjustments are based on just a few BG values from meals, it can be very challenging to achieve good BG control [ 7 ]. In reviewing BG data and trend patterns, providers and patients ideally collaborate to make decisions about the adequacy of dosing and timing of insulin, exercise, and diet, in order to educate the patient, incorporate important individual information, and tailor the best approach for each individual person.
One impediment to using BG data in patient education is access to the BG data itself. Behavioral and technical issues negatively influence both patient and clinician access to timely and complete BG data. Missing values may be related to a person’s psychosocial issues, health literacy, or disengagement with one’s health [ 8 , 9 ]. Missing values may provide a focus point for improving adherence, but interfere with pattern recognition and prevent fully informed decision-making. Polonsky et al found that in adults with T2D many insulin users (42%) and noninsulin users (50%) do not bring self-monitored blood glucose (SMBG) data regularly to medical visits [ 9 ]. Because there is still controversy surrounding the utility of SMBG in people with T2D who are not taking insulin [ 5 ], some of these people may have less motivation to continue to monitor their BG values due to conflicting recommendations. In a study by Farmer et al of that followed 453 people with non- insulin treated T2D, no additional benefit was found in the non-insulin treated T2D participants who monitored their BG compared to controls that did not monitor their BG [ 10 ]. A limitation of this study was that it was unclear what education took place around the BG values obtained by the participants [ 5 ]. But overall, unlike a person on insulin who can take direct actions to mitigate a BG reading that is out of range, the options available to people with T2D not taking insulin are less immediately impactful and include adjustment of their diet and exercise regimens, and speaking to their physicians about adjusting oral medications. While these actions can impact the person’s glycemic control, their connections to BG values are not immediate or readily apparent. Finally, economic factors may also pose a barrier to multiple daily BG monitoring in T2D due to the high cost of BG strips, and the reality that insurance companies generally limit the amount of strips covered in people with T2D [ 11 ].
Even in people with T1D, however, where there is a direct connection with BG values and subsequent actionable steps that can be taken, psychosocial barriers to monitoring BG values such as motivation, anxiety, and perceived susceptibility can also impact the person’s willingness to monitor. Although a person may perceive that they are engaging in all the steps required of them to monitor their BG, calculate their insulin dose and sliding scale, and administer insulin, they may still have BG values that do not reflect their effort and planning because of other external factors like stress, illness, exercise, puberty, and other hormones that can affect BGs [ 12 – 15 ]. Perceived and real lack of control can be demotivating and lead to decreased self-efficacy, which may affect a person’s willingness to continue checking their BGs [ 16 ]. In youth, a lack of perceived susceptibility risk to the long term consequences of poor management may lead to further lack of motivation for BG monitoring [ 17 ]. In all ages of T1D and T2D, anxiety over glycemic variability may further dissuade people from BG monitoring and lead to more missed values [ 18 , 19 ]. While BG technologies, such as continuous glucose monitoring (CGM), may help with these missing values by providing multiple readings per hour, if a person is still not checking regularly to calibrate a CGM, the output itself will not be reliable [ 20 ]. Finally, other psychosocial obstacles to BG monitoring such as inadequate numeracy may serve as barriers that may influence a person’s willingness to monitor their BG values [ 21 ]. If a person does not feel confident interpreting the numeric values they obtained from self-monitoring, they will not likely recognize the value in monitoring BG values.
Once BG values are appropriately obtained, a person must be educated about and carry out several steps in the problem solving pathway such as interpreting the value, problem solving around the BG data, making adjustments to their regimen based on the data, and iterating the process several times through each day in order to maintain glycemic control. Many studies have tested a variety of clinical and behavioral approaches for improving glycemic control in people with T1D and T2D. However, we were specifically interested in understanding how blood glucose values obtained from people with diabetes have been integrated into patient education and support programs within the research literature. Here, we review intervention studies to identify the frequency that BG values have been the focus of patient education research and the nature of those interventions designed to improve glycemic control. Specifically, we sought to characterize the use of different methods to integrate BG into an intervention, the approaches implemented to support patient education and behavior change, and the nature of communication about BG values.
Data Sources
The search strategy focused on MEDLINE for eligible articles using a combination of the following key words “education”, “teaching”, “blood glucose”, “glucose value”, “interpretation”, “intervention”, each crossed with the term diabetes mellitus . In addition, we contacted experts in the field to identify studies, and hand-searched references of key articles.
Inclusion and Exclusion Criteria
No limitations of publication date were used in the search. Articles that did not use blood glucose values for education, tested interventions but did not discuss how the values were obtained or used, or were not published in English were excluded from the review.

Study Selection and Data Extraction
The full text of potentially eligible articles was examined to determine whether they contained relevant information. One investigator (YKC) initially abstracted information from the articles, then both investigators reviewed articles together. Any discrepancies between the initial review and combined review were resolved through discussion and reference to the original articles. Thirty-four eligible studies were identified that included patient education using BG values. Information regarding the study and intervention characteristics include: 1) Characteristics of the study sample, 2) How BG values were obtained, 3) Use of a graphical interface for BG values, 4) Use of a BG log, 5) BG interpretation and regimen adjustments, 6) Recommended actions to patient, 7) Modality of intervention, and 8) Intervention communication schedule.
Table 1 lists the studies and their characteristics. Of the 34 studies reviewed 21 (62%) focused on T1D and 13 studies (38%) focused on T2D. The age range of participants with T1D in these studies varied from 5 to 58. The age range of the participants with T2D ranged from 18 to 72. The studies that included people with T2D were managed with diet alone, diet and oral medications, or diet, oral medications and insulin.
Study Characteristics of Interventions Using Blood Glucose Data in Patient Education
| Author (Year) | T1 or T2 | Pediatric or Adult Participants | Number of Intervention Participants | How BG Values Were Obtained | Graphical Interface for BG Values | Log of BG Values | BG Interpretation & Regimen Adjustments | Recommended Actions to Patient | Mechanism of Intervention | Intervention Schedule |
|---|---|---|---|---|---|---|---|---|---|---|
| T2 | Adult | 14 | Semi-automated: CGM uploaded | Yes | Yes | Patient + Provider | Lifestyle | Phone | Monthly | |
| T1 | Adult | 15 | Semi-automated | No | No | Provider | Dosing | SMS | Weekly | |
| T1 | Pediatric | 14 | Semi-automated | No | No | Provider + Program | Dosing | Phone | 2 Weeks | |
| T1 | Pediatric | 30 | Semi-automated | No | No | Provider | Dosing + Lifestyle | Phone | 2 Weeks | |
| T2 | Adult | 34 | Semi-automated | No | No | Provider | Dosing + Lifestyle | SMS | Bi-weekly | |
| T1 | Adult | 17 | Manual: Logbook | Yes | Yes | Patient | Monitoring | Internet | Multiple times a day | |
| T2 | Adult | 15 | Semi-automated | No | No | Program | Dosing + Lifestyle | SMS | Daily | |
| T1 | Adult | 47 | Semi-automated | Yes | Yes | Provider | Dosing | Phone | Weekly | |
| T1 | Pediatric | 12 | Semi-automated | No | No | Provider | Dosing + Lifestyle | SMS | 3 Days | |
| T1 | Pediatric | 50 | Semi-automated | No | No | Provider | Dosing | Phone, Letter | 2 Weeks | |
| T1 | Pediatric + Adult | 22 | Semi-automated | No | Yes | Program | Follow Regimen | SMS | Weekly then Monthly | |
| T1 | Adult | 74 | Semi-automated | No | Yes | Patient | Dosing + Lifestyle | In Person | Weekly | |
| T1 | Pediatric | 47 | Semi-automated | No | No | Patient + Provider | Dosing | Phone | 2 Weeks | |
| T2 + | Adult | 72 | Semi-automated | No | No | Provider | Unclear | Letter | Unclear | |
| T1 | Pediatric | 23 | Semi-automated | Yes | No | Provider | Dosing | In Person | Monthly | |
| T2 + | Adult | 47 | Semi-automated | Yes | No | Program | Dosing | SMS | 3 Days | |
| T2 + | Adult | 18 | Semi-automated | No | No | Provider | Dosing + Lifestyle | SMS | Weekly | |
| T2 + | Adult | 33 | Semi-automated | No | No | Provider | Dosing | SMS, Internet | Weekly | |
| T1 | Adult | 10 | Semi-automated | Yes | Yes | Program | Dosing | SMS | Multiple times a day | |
| T2 + | Adult | 185 | Manual: SMS | Yes | Yes | Provider | Dosing + Lifestyle | SMS | Unclear | |
| T1 | Pediatric | 23 | Semi-automated | No | No | Provider | Dosing | Phone | Weekly | |
| T2 + | Adult | 8 | Semi-automated | Yes | Yes | Provider | Dosing | At Will | ||
| T1 | Pediatric | 52 | Semi-automated | No | No | Provider | Dosing | Phone | 2 Weeks | |
| T1 | Pediatric | 60 | Semi-automated | No | No | Provider | Dosing + Lifestyle | Phone | 3 times a week | |
| T1 | Pediatric | 25 | Manual: Voice | No | Yes | Provider | Dosing | Phone | Weekly | |
| T2 | Adult | 256 | Manual: Logbook | No | Yes | Patient + Provider | Dosing + Lifestyle | In Person | 3 Months | |
| T2 + | Adult | 13 | Semi-automated | No | Yes | Program | Dosing + Lifestyle | SMS | 2 Weeks | |
| T1 | Pediatric | 18 | Semi-automated | No | No | Provider + Program | Dosing | SMS | Weekly | |
| T1 | Adult | 67 | Manual: SMS | No | No | Program | Dosing | SMS | 2 Times a Week | |
| T1 | Parents | 16 | None | No | No | Patient | Dosing + Lifestyle | In Person | Once time | |
| T1 | Adult | 102 | Manual: SMS | No | No | Provider | Dosing +Monitoring | SMS | Weekly | |
| T1 | Pediatric | 47 | Manual: Logbook | No | Yes | Patient | Dosing + Lifestyle | Self | Monthly | |
| T2 | Adult | 57 | Semi-automated | No | No | Program | Lifestyle | SMS, Internet | Multiple times a day | |
| T2 + | Adult | 25 | Semi-automated | Yes | Unclear | Provider | Dosing + Lifestyle | SMS | Weekly |
How Blood Glucose Values Were Obtained
The first and most critical step in providing BG education and support is to reliably and regularly obtain that data. In these studies, BG values were obtained using a variety of methods, including traditional hand written log books and more recently developed methods such as automated uploads from wireless meters. The methods that BG values were obtained and delivered for further analysis were characterized as manual or semi-automated. No fully automated BG systems were utilized in these studies.
Approximately 24% of studies utilized some form of patient-dependent manual entry of BG values. Manual entries of BG data included hand recording of BG values into logbooks or into a computer website [ 22 – 24 ], providing the BG values by voice over a telephone to a designated person who would then record them [ 25 ], or sending the values via short message service texting (SMS) on a mobile phone [ 26 – 28 ].
Approximately 76% of studies used semi-automated methods for obtaining BG values. Semiautomated methods were defined as those that involved automation of uploading or transfer of the values into an electronic database or system. The semi-automated systems varied in the extent to which participants had to initiate actions in order for the BG values to be integrated into the systems. Semiautomated systems either 1) transmitted BG data wirelessly via Bluetooth or infrared after some minor action from the participant such as transmitting the values from a meter to a phone or PDA [ 29 – 32 ] or 2) required the participant to upload their meter through a hard-wired connection to a phone or computer where the information would then be sent to a server and/or downloaded within a clinic setting [ 33 – 39 ].
Blood Glucose Interpretation
Display and summarization of bg values.
A potentially impactful tool related to BG education is the use of graphical displays of values over time. This critical element of clinical management and patient education allows more efficient pattern recognition and problem solving. Meters and pumps often provide software that will aggregate BG values over time to identify salient patterns and values that are out of range. Within these intervention studies, 9 (26%) provided a graphical display of data for the participants [ 22 , 28 , 29 , 33 , 39 – 43 ]. By having graphical data available for view by the participant, the studies could provide another dimension for BG data interpretation.
It was unclear in most studies whether viewing the graphs was a mandatory part of the intervention. The study by Allen et al (2011) using continuous blood glucose monitoring (CGM) did require that the graphical display was viewed and utilized for patient education [ 43 ]. Allen et al evaluated the impact of problem solving on physical activity. Participants with T2D received a 90-min CGM education session provided by a certified diabetes educator. Data from the CGM were used to tailor the intervention about the effects of physical activity on each participant’s blood glucose levels. Color graphs and summary tables were used along with participants’ logged events such as meals, medications, and stress to aid in interpreting glucose values. The results indicated improved problem solving skills in the intervention group with continuous glucose monitoring plus problem solving compared to a control group of continuous glucose monitoring plus just general education [ 43 ].
Participant and Provider Roles
Once BG values are obtained, they are ideally interpreted in the context of the participant’s behaviors such as carbohydrate intake, appropriate dosing, and treatment goals. Interpretation, problem solving, decision making around BG values took three general forms in the research. Within these interventions: (1) the participant interpreted the values independently (11% of studies) [ 22 , 23 , 44 •, 45 ], (2) the participant interpreted the BG values with providers support (9% of studies) [ 24 , 43 , 46 ] or (3) most frequently, the provider or an automated program interpreted the BG values alone and communicated instructions to the participant (80% of studies ) [ 25 – 42 , 47 , 48 ••, 49 – 55 ].
Recommended Actions
The types of decisions that were recommended after the values had been obtained and interpreted depended on the type of diabetes under study. Intervention components included options such as behavior change, medication management, or insulin management. The recommendations made were either to adjust insulin dose or diet and exercise or both. In interventions that just included participants with T2D that were not on insulin, the regimen adjustments included recommendations for lifestyle modifications such as diet or exercise behaviors [ 43 , 48 ], and dosing adjustments of oral medications [ 24 , 37 , 52 ]. Additional recommendations for participants with T2D also on insulin would include adjustments to the insulin regimen as well [ 28 , 29 , 32 , 33 , 42 , 49 , 53 , 54 ]. In the T1D studies the intervention recommendations mostly involved just insulin adjustment suggestions [ 25 , 26 , 30 , 34 , 36 , 38 – 41 , 46 , 50 , 55 ]. Some studies also included suggestions to modify diet and exercise, which is a good overall approach to help the participants understand the full picture of the multiple factors that play into their management [ 23 , 31 , 35 , 44 , 45 , 51 ].
Polonsky et al (2011) provide a good example of an intervention designed to engage people with diabetes in the interpretation of their own BG values. In this 12-month, cluster-randomized clinical trial, insulin naive adults with T2D were randomized to an intervention of collaborative, structured glucose monitoring or no structured monitoring. The experimental group utilized a paper tool that was used to record a 7-point self-monitoring blood glucose (SMBG) profile for three consecutive days prior to their quarterly physician visit. The participants were taught to interpret their own SMBG results and would bring the completed form to their physician visit. Each profile included space to record pre-prandial and post-prandial BG values at each meal and at bedtime, plus ratings of meal size and energy level to enhance visualization of patterns. Participants and physicians interpreted SMBG results together to make medication and lifestyle changes. Intervention participants displayed significantly greater reductions in distress related to regimen adherence than controls and a greater reduction in glycemic control [ 24 , 56 ] [ 57 ]. This structured SMBG monitoring also led to significant increases in self-confidence and autonomous motivation associated with diabetes self-management [ 58 ].
Sullivan-Bolyai et al (2012), incorporated parents in the interpretation of BG values, with a pilot study to test the use of pediatric human patient simulators to teach parents diabetes management for children newly diagnosed with T1D. Participants received standard hypoglycemia education using vignettes and pediatric simulations to illustrate care. The teaching sessions included review of glucose monitoring, daytime and nighttime hypoglycemia, drawing up and administering insulin and glucagon, and observation and treatment of tremor and seizure activity. Focus group participants enthusiastically supported the use of the pediatric simulated patients after diagnosis for the education of hypoglycemia and also to focus on more complex diabetes management concepts [ 44 ].
Intervention Communication Characteristics
The frequency of communication with participants in the studies varied widely from multiple times a day [ 22 , 41 , 48 ] to monthly [ 23 , 39 , 43 ]. Modalities that were automated to give feedback generally had more frequent communication than modalities that required face to face or clinician contact [ 37 , 41 , 48 ].
Modality of Intervention Communication
In addition to how the BG data was obtained, displayed, and interpreted, we identified predominant methods by which the participants communicated with the interventions: these methods included email [ 29 ], in person communication with the intervention group [ 24 , 39 , 44 , 45 ], phone [ 25 , 34 – 36 , 38 , 40 , 43 , 46 , 50 , 51 ], SMS [ 26 – 28 , 30 , 31 , 33 , 37 , 41 , 42 , 47 – 49 , 52 – 55 ], Internet [ 22 ], and letters [ 32 ].
One study utilized a novel multi-modal approach to communication. A study by Froisland et al (2012) sought to improve diabetes care for young people with T1D through visual learning on mobile phones. The intervention used an application that contained a picture-based diabetes diary to record physical activity and photos taken with the phone camera of food eaten, where the phone also communicated with the glucometer by Bluetooth technology to capture blood glucose values, and a Web-based SMS where participants could send messages to their providers when they faced obstacles, and also could receive educational messages. At the end of the study, participants reported an increased understanding of applied knowledge of self-management with associated improvement in diabetes self-care, and reported that SMS gave them a feeling of increased access and security [ 31 ].
Improving the frequency of communication was evident in most of the studies. In a study of adults with T2D by Yoo et al.(2009) participants in the intervention groups received a cellular phone with a modular blood glucose measuring device which reminded the participant to measure their blood glucose twice a day, and would also remind them to measure blood pressure and body weight. As soon as the participants transmitted their glucose measurement through their phones, they would immediately receive messages of encouragement, reminders, and recommendations for lifestyle changes from a pre-defined algorithm developed by an endocrinologist. After the 12 week intervention the study found significant reduction in A1C in the control group compared to the intervention group, and significant improvement in additional parameters such as blood pressure and cholesterol in the intervention group.
A review of relevant research indicated that interventions primarily incorporated methods to improve clinician access to BG data, to improve the frequency of communication with participants, and to provide regimen adjustments for participants required to improve their diabetes management. There was no predominant approach to implementing these processes. Many systems sought to provide advice to participants regarding insulin dosing around a specific BG value, but did not educate or engage the participants in the process of discovery and problem solving around their BG values.
There was a wide range of approaches to obtaining BG values, ranging from traditional paper log books to semi-automated wireless systems. One potential value of using manual BG collection methods is that the act of recording or stating the values may bring awareness to specific high or low values. However, manual delivery of BG values may lead to more missing data, data entry errors, and recall bias if not looking at a meter. Another potential disadvantage of manual BG entry is that it may lead to disengagement if a person feels burdened by repetitive entry of their data. Recent advances in the integration of the Internet and wireless technologies have changed the nature of this process and provided much greater access to BG data for people with diabetes and their providers. Integrating meter-uploaded data within clinical research may reduce missing values, enhance data reliability, allow real-time or near real-time support, and provide the quantity of data needed to examine trends over longer periods of time. Although currently available, we could not identify any fully automated BG transmission systems. All systems required the participants to take additional steps beyond monitoring their BG in order to transmit their information.
Regardless of the method of obtaining BG data, interpretation and the ability to identify patterns and make actionable insights can be enhanced through data visualization techniques. Approximately one quarter of the interventions described using a graphical BG display. However, it was often unclear how data was displayed, what specifically was displayed, or how the graphical display was used for the provider or the participant. Graphical displays are able to provide a richer understanding of data, but just as easily could lead to confusion for people unfamiliar with that modality of communication. Graphical communication, and its integration with verbal and written materials, are unexplored areas of patient BG education.
Some of the technological solutions discussed above reduce barriers to BG monitoring, such as numeracy, by directly calculating and recommending regimen changes based on the person’s BG so that no additional calculations are required. While this technical advance may be helpful, it may not directly contribute to improvement in a person’s understanding of the relationships involved or support self-efficacy in order to empower future self-management decision-making.
Although recommended by professional diabetes organizations like the ADA [ 59 ], and integrated in some studies here, collaborative problem solving and goal setting were not commonly utilized. Blood glucose values were utilized primarily by clinicians or automated systems to make unilateral insulin dosing adjustments. Automated response technologies facilitate dosing decisions and likely lead to more accurate dosing. However, those systems and the associated studies, typically did not seek to influence or indicate gains in participant knowledge, or understanding of the relationships between BG, exercise, and diet. Blood glucose data needs to be interpreted within the context of data related to these important self-management behaviors. Missing blood glucose values also need to be examined within the context of psychosocial and behavioral influences.
The most variable aspect of the research was observed in the communication modalities and frequencies between participants and either providers or a “system.” Due to highly variable reporting, the relation between communication frequency and participant attrition or missing BG data was not clear. Because many of the studies focused on mobile technology, the communication tended to take place using SMS or real-time phone calls. More research focused on the frequency and modality of communication around BG data is needed, specifically, how to identify triggers and thresholds for different types of communications.
While data supports the important role of monitoring BG values in people with diabetes, there is a disconnect between the recommended guidelines for BG monitoring frequency, the technological tools available to people with diabetes and the provider's ability to facilitate the process, and what is actually being done. The technologies discussed above do not address barriers such as understanding relationships between BG and insulin dose, adherence problem solving skills, insurance limitations, or self-efficacy. There was a lack of focus on missing BG values, with the assumption that a person with diabetes is generally taking the key steps to obtain their BG values. A primary focus of the studies was on transmitting the BG values to providers who would then specify solutions to the participants.
The interventions tested within many studies were in their initial developmental stage, with no data on implementation. Moving forward, the feasibility of such systems should be taken into account as incorporation of many of the technologies and systems described may be cost prohibitive for clinicians to set up and patients to use on a regular basis. Even with the basic technologies like phone support and simple SMS texting that are readily available, the resource demands to integrate that data into clinical informatics systems and maintain them may be difficult without an existing provider compensation model to justify the additional time and expense. While the data may show that incorporation of these tools may be of some benefit, the evidence may not be overwhelming enough for providers to justify the investment in their current health infrastructure.
The research demonstrates that new BG technologies provide outstanding opportunities for greater access to BG data and intervention focuses for people with diabetes. However, the research also points to the need to improve and expand our education and support for people in their daily use of BG values to maintain and improve glycemic control. In order to make the most sustainable impact on people’s self management behaviors, barriers to obtaining BGs must be addressed, generalizable skills such as problem solving need to be integrated into patient BG education, and resources to support the use of these tools should be identified to help facilitate their integration into routine clinical care.
Conflict of Interest
Yaa Kumah-Crystal and Shelagh Mulvaney declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Yaa Kumah-Crystal, Vanderbilt University Medical Center, Department of Pediatrics, Monroe Carell Jr. Children’s Hospital at Vanderbilt, 2200 Children’s Way DOT Room 11142-C, Nashville, TN 37232-9170.
Shelagh Mulvaney, Vanderbilt University Medical Center, School of Nursing, Department of Pediatrics, & Department of Biomedical Informatics, 461 21st Avenue South, Nashville, TN 37240.
- Research article
- Open access
- Published: 04 May 2016
Systematic literature review of use of blood glucose monitoring in phase III clinical studies of insulin analogs
- Kaisa Miikkulainen 1 ,
- Antonio Caruso 2 ,
- Oliver Mast 3 ,
- Rongrong Zhang 1 &
- Oleg Borisenko 1
BMC Endocrine Disorders volume 16 , Article number: 21 ( 2016 ) Cite this article
4223 Accesses
4 Citations
Metrics details
Safe and effective insulin therapy for diabetes mellitus requires initial dose titration and regular adjustments based on blood glucose (BG) monitoring. Our objective was to explore the use of BG measurement in phase-III clinical studies of insulin analogs. These studies provide safety and efficacy information for regulatory authorities and are the basis for insulin analog regulatory approval.
A systematic review of phase-III studies of rapid-acting insulin analogs (insulin lispro, insulin aspart and insulin glulisine) and pre-mixed insulin analogs (biphasic insulin aspart and insulin lispro mix) was conducted. Studies were identified using manufacturers’ databases. Search for reports was performed in Medline and registry of clinical trials (clinicaltrials.gov). The European Medicines Agency was contacted to provide Clinical Study Reports.
Forty-five studies were included. Regular BG measurements were reported in 100 % of the studies and were performed by either self-monitoring of blood glucose (SMBG) alone in 84 %, laboratory alone in 7 %, and both SMBG and laboratory in 9 % of studies. In total, 93 % of the studies reported SMBG. Most studies (91 %) reported insulin therapy adjustments based on BG measurements.
Conclusions
The findings suggest that BG monitoring and specifically SMBG are co-dependent technologies with insulin analogs. BG measurement is used in most phase-III registration studies for establishing safe and efficacious insulin administration and is recommended in the insulin labels. The indispensable role of SMBG in treatment of insulin-dependent patients should receive attention from health care payers to assess and reimburse SMBG along with insulin to avoid adverse events from inappropriate insulin administration and associated costs.
Peer Review reports
Multiple stakeholders, including regulatory authorities, clinicians, payers (commissioners) and health technology assessors, are involved in market introduction and management pathways for health technologies. From the perspective of these stakeholders, monitoring of blood glucose (BG) in insulin-dependent diabetes has strong global support from clinical societies [ 1 – 6 ]. The American Diabetes Association guidelines specify that “major clinical trials of insulin-treated patients that demonstrated the benefits of intensive glycemic control on diabetes complications have included self-monitoring of blood glucose (SMBG) as part of multifactorial interventions, suggesting that SMBG is a component of effective therapy” [ 1 ]. Regulatory authorities have approved the use of blood glucose meters for use with insulin products and have outlined instructions for the measurement of BG [ 7 ]. Health technology assessments, although rarely focused on SMBG in insulin-dependent diabetes, have also been in general supportive of BG monitoring [ 8 , 9 ]. Lack of understanding of the role of BG monitoring in the safe and effective use of insulin leads to restrictions or no coverage of SMBG in some developing countries, while reimbursement for insulin treatment is provided [ 10 ]. According to Czupryniak et al. [ 11 ], access to SMBG is limited especially in Central and Eastern European countries. In a survey conducted in 47 countries by the International Diabetes Federation, existing limitations for access to SMBG were also confirmed [ 12 ]. Limitations usually do not have rational ground and can mainly be explained by the absence of a consistent reimbursement system. Another potential reason for restrictions of SMBG is the lack of randomized controlled trials (RCTs) for comparing the management of insulin-dependent diabetes with and without SMBG. RCTs are considered as a “gold standard” for assessment of safety and efficacy of health care interventions [ 13 ], although their role in assessment of effectiveness of SMBG as stand-alone technology can be reasonably questioned. The role of SMBG in insulin-dependent diabetes has not been studied in RCTs and does not require validation in comparative studies, as it would be considered unethical to allocate patients to insulin without the ability to determine and adjust dose based on BG measurements. Another contributing factor to complexity of assessment of efficacy of SMBG is that is it a diagnostic measure, not a treatment intervention.
SMBG and the use of insulin are ultimately linked together for an effective and safe therapy. Regulatory approval of insulin has been established in phase III clinical studies [ 14 ]. Because BG is an essential component of these foundational studies of the safety and efficacy of insulin treatment, it provides additional arguments for the use of SMBG, and thus confirms the co-dependent nature of SMBG and insulin treatment. Therefore, it is necessary to consider them jointly in evidence evaluations and reimbursement decision making, and BG monitoring should be mentioned as a part of the intervention in the studies on insulin analogs.
In a preliminary review of phase III clinical studies of insulin analogs, it was found that in only 12 of the 57 study synopses analyzed, dose adjustments were made according to BG measurements [ 7 ]. In addition, full text reports were not available for review in most of the studies. Our study aimed to explore this area further, and we hypothesized that phase III registration studies of commonly used insulin analogs (biphasic insulin aspart, insulin aspart, insulin glulisine, insulin lispro and insulin lispro mix) include BG monitoring and consequent regular dose adjustment as an essential element of the research protocol. The resulting impact on the treatment outcomes is thought to be a joint effect of the co-dependent technologies.
A systematic literature review was performed in multiple steps. First, a systematic search for phase III clinical studies was performed on the manufacturers’ websites (Novo Nordisk A/S, Eli Lilly and Company, Sanofi S.A.). The rapid-acting insulin analogs included insulin aspart (NovoRapid®), insulin glulisine (Apidra®) and insulin lispro (Humalog®). Pre-mixed insulin analogs included biphasic insulin aspart (Novo Mix®) and insulin lispro mix (Humalog Mix®). All searches were conducted in December 2013. Second, Clinical Study Reports were requested from the European Medicines Agency (EMA), according to Regulation (EC) No 1049/2001. Third, an additional search for full-text publications was performed in Medline and Medline In-Process bibliographic databases using the clinicaltrials.gov identification number (clinical trial ID) or the manufacturer’s study ID. If no full-text publication was identified in the bibliographic databases, a search was performed in the registry of clinical studies clinicaltrial.gov. Finally, a study synopsis or summary was retrieved from the manufacturers’ websites. Only prospective phase III clinical trials of insulin analogs that reported clinical outcomes were included, as insulin analogs (in comparison with human insulin) are more recently available and have followed the most recent regulatory procedures.
Data collected included country of origin, design of the study, sample size, mean age, type of diabetes, duration of diabetes, proportion of males, use of insulin before enrollment into study, target glycated hemoglobin (HbA1c) in the inclusion and exclusion criteria, mean HbA1c, use and purpose of BG measurement, method of insulin dose adjustment, structuration of SMBG, provision of education/training for SMBG, and monitoring of compliance in SMBG. The data were extracted by one reviewer and validated by a second reviewer. Any disagreements were resolved by consensus. No statistical hypothesis was tested. The main outcomes included frequency of use of BG monitoring and use of BG monitoring for insulin dose adjustment. Summary statistics were provided using SPSS version 20 (IBM Corp., Armonk, New York, USA). Study did not require ethical approval, as it did not include any patient’s data.
Clinical studies search
Altogether 46 phase III clinical trials were identified in the manufacturers’ websites. One retrospective study (NCT00410033) was excluded from analysis, as it did not meet inclusion criteria. The database search in Medline provided 27 full-text articles, one of which was identified as a duplicate [ 15 ] and five as redundant publications [ 16 – 20 ]. All five redundant publications were considered less informative than the main published phase III clinical study in question. EMA provided eight out of the 45 requested extracts of Clinical Study Reports of the phase III insulin analog studies. The majority of the Clinical Study Reports were not held by EMA. The analog reports which were provided consisted of the following: insulin glulisine ( n = 1), biphasic insulin aspart ( n = 3) and insulin lispro ( n = 4). For three studies, both the Clinical Study Reports and full-text publications were available, but for five studies, only the Clinical Study Report was available. A detailed description of the selection process as adapted from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework [ 21 ] is presented in Fig. 1 .
Selection of phase III trials and subsequent full-text publications (adapted from PRISMA [ 21 ])
Description of included studies
The characteristics of the included studies are described in Table 1 . Of the identified phase III studies, 62 % ( n = 28) were rapid-acting insulin analog studies and 38 % ( n = 17) were pre-mixed insulin analog studies. Of the rapid-acting analogs, 29 % ( n = 8) were insulin aspart, 57 % ( n = 16) were insulin glulisine and 14 % ( n = 4) were insulin lispro. Of the pre-mixed insulin analog studies, 71 % ( n = 12) were biphasic insulin aspart studies and 29 % ( n = 5) insulin lispro mix studies.
The majority ( n = 40, 89 %) of the included studies were RCTs. In total 60 % ( n = 27) were single-country studies conducted in USA ( n = 9, 20 %), Japan ( n = 5, 11 %), China ( n = 3, 7 %), Russia ( n = 2, 5 %), and 1 ( n = 1, 2 %) each in Germany, Denmark, Italy, France, Mexico, the Netherlands and Ukraine. There were 29 % ( n = 13) of the studies conducted in multiple countries; the location was not specified in 14 % ( n = 6) of the studies. The median number of patients in the studies was 280 (interquartile range 113–403).
Type 1 diabetes mellitus (DM) patients were included in 31 % ( n = 14) and type 2 DM patients in 51 % ( n = 23) of the studies. A mixed population consisting of patients with both type 1 and 2 DM was identified in 16 % ( n = 7) of the studies. One study included patients with gestational DM only.
In 89 % ( n = 40) of the studies, only adults were included, and in 7 % ( n = 3) only children and/or adolescents were included. In two (4 %) studies, the patient population was mixed where both adults and children were included. Mean age of patients in all studies was 48.3 (standard deviation [SD] 14.6) years. Males constituted on average 53 % of all study participants. The mean duration of diabetes prior to enrolment was 12.2 (SD 4.6) years and insulin therapy had been initiated prior to enrolment in 78 % of the studies. Patients had not received insulin therapy prior to enrolment in 13 % of the studies. The mean level of HbA1c at baseline was 8.3 % (SD 0.9 %).
BG monitoring in the included studies
Bg monitoring.
A summary of the results is presented in Table 2 . Regular monitoring of BG was reported in 100 % ( n = 45) of the studies as shown in Fig. 2 .
Proportion of phase III clinical trials that reported regular BG monitoring per insulin analog type
Insulin doses were reportedly adjusted based on regular BG measurements in 91 % of phase III studies (Fig. 3 ). In total 31.1 % the studies were with patients making insulin dose adjustments using BG values. Physician-adjusted insulin dosing using BG values was reported in 37.8 % of the clinical studies that reported BG monitoring. In 4.4 % of the studies dose adjustment was reported by both patients and physicians. In 18 % of the studies, dose adjustment based on BG values was performed, but it was not specified by whom.
Proportion of phase III trials reporting insulin dose adjustments
SMBG monitoring
SMBG was reported in 93 % ( n = 42) of the phase III clinical studies. The proportions of studies using either rapid-acting or pre-mixed insulin analogs were similar in terms of those reporting SMBG. SMBG was used as the only means of BG monitoring in 84 % ( n = 38) of the studies. Monitoring of BG using only laboratory means was reported in 7 % ( n = 3) of the studies. Both laboratory and SMBG measurements were reported in 9 % ( n = 4) of the studies.
With regard to insulin dose adjustments based on SMBG, 33.3 % ( n = 14) of the phase III clinical studies reported that patients self-adjusted insulin doses based on SMBG results. The proportion of these studies using either rapid-acting ( n = 9, 34.6 %) or pre-mixed insulin ( n = 5, 31.3 %) was the same. Adjustment of insulin doses by physicians based on SMBG values were reported in 38.1 % ( n = 16) of the studies. Dose adjustment by physicians based on SMBG was similar in the pre-mixed ( n = 6, 37.5 %) and the rapid-acting insulin analog ( n = 10, 38.5 %) studies. In two studies (4.8 %) SMBG-based dose adjustments were reported both by patients and physicians. In four (9.5 %) studies that reported dose adjustments based on SMBG, it could not be determined whether the dose adjustments were carried out by physician or patient.
Daily frequencies of SMBG measurement were reported in 83 % ( n = 35) of the studies that reported the use of SMBG. In general, the daily frequencies varied between one to nine tests.
Training, education and provision of instructions for the proper use of SMBG were reported in 55 % ( n = 23) of the phase III studies where SMBG was reported. Monitoring the proper use of SMBG was reported in 64 % ( n = 27) of the studies that reported SMBG measurements. The monitoring was frequently done by regular checks via telephone and by inspecting patient diaries.
To our knowledge, the present study is the first to systematically assess the role of SMBG in phase III clinical studies. It confirms the role of BG measurement as an essential component of safe and effective insulin therapy. We found that in 100 % of phase-III clinical studies of analog insulins, BG monitoring was regularly used. SMBG was the most prevalent monitoring option and was reported in 93 % of the studies.
We also found that in the majority of the studies insulin therapy was regularly adjusted based on the BG measurements. Therefore, the safety and efficacy of insulin use requires guidance for patients in the use of BG measurements and the corresponding dose adjustments. Of the studies reporting BG use, 31 % included insulin dose self-adjustment by patients, 38 % with dose adjustment by physicians, 4 % with dose adjustment by both patients and physicians and finally 18 % in which dose adjustment was performed, but it was not reported by whom. For the other studies that did not explicitly mention insulin dose adjustment based on BG measurement, we cannot rule out that dose adjustment did not occur. However, all these studies were unpublished and no Clinical Study Reports were available. If the analysis is limited only to the studies for which either full text publication or the Clinical Study Report is available, then insulin dose adjustment based on BG measurements would be in 100 % of the studies, both for rapid-acting and pre-mixed insulins.
Our analysis also showed that only 55 % of the examined studies report that training, education or provision of instructions about the use of SMBG took place. We believe that this relatively low value reflects incomplete reporting in the studies, rather than a lack of provision of training. Studies have demonstrated that structured testing can enhance the value of SMBG [ 22 – 24 ]. Structured testing means measuring BG at specific times or in relation to activities in order to best evaluate the effect of therapy, diet and physical activity on the BG level [ 25 ]. In a review of the European Public Assessment Reports for insulin analogs, it was revealed that unspecific and unclear recommendations for BG monitoring is occasionally provided [ 7 ]. To ensure safe and effective use of insulin, manufacturers should be encouraged to provide clearer recommendations for patients and medical professionals.
This study contributes to the understanding of the essential role of BG monitoring in insulin-dependent diabetes. Insulin is safe and effective if used only in combination with regular BG monitoring. This is true for both rapid-acting and pre-mixed insulins, the latter typically used in conventional insulin therapy. The value of BG monitoring is for providing essential information for making therapeutic choices, either by the patient or the physician. And SMBG is only helpful, if it results in therapeutic consequences. To achieve that SMBG shall be placed in the center of the disease management for diabetic patients, including appropriate training of structured testing, as mentioned above. The use of both SMBG and insulin is funded in the majority of developed countries by payers. In some developing countries, reimbursement is not available for BG meters and strips, while coverage for insulin treatment is provided. The lack of affordability or reimbursement limitations of SMBG may impair adherence to the recommended BG test frequencies and result in not achieving the required level of efficacy and safety of insulin, which could ultimately lead to adverse outcomes for the patients and an increase in cost to the health care system due to ineffective management of diabetes.
Data on the impact of non-provision of SMBG on insulin-dependent patients are limited, although some emerging evidence shows a potential serious risk of a reduction of insulin effectiveness. In China, where SMBG is not reimbursed, a study in 2011 with 10,418 patients with diabetes revealed that a high proportion of insulin-dependent patients do not have a meter at home to perform SMBG (51.6 % of patients on intensive insulin therapy, 46.6 % on conventional insulin therapy and 39.9 % on basal-supported oral therapy) [ 26 ]. In all three of these clinical groups, the average level of HbA1c was higher in patients who did not have access to a SMBG meter (e.g., HbA1c 8.1 % with SMBG vs HbA1c 9.3 % without SMBG among patients on intensive insulin therapy). In another study from India ( n = 2250) using a similar study methodology as in the study in China of accessibility to SMBG, it was found that 41.5 % of patients on intensive insulin therapy, 54.3 % on conventional insulin therapy and 44.6 % on basal-supported oral therapy did not have a meter at home to perform SMBG [ 27 ]. The level of glycemic control was lower in patients who did not perform SMBG. In a study performed in Italy, it was demonstrated that patients using SMBG had a reduced risk of diabetes-related hospitalizations and consequently a lower overall total annual cost per patient [ 28 ]. Total annual cost was €3060 in the group of no SMBG users vs. €2738 in the group of patients using SMBG, which was mainly explained by statistically significant reduction of diabetes-related hospitalizations.
Non-coverage of SMBG in some developing countries is a good example of ‘silo budgeting’ to overcome, when different payers are responsible for provision of drugs and diagnostics/medical aids. Being disconnected, the decision-making and financial flows for drugs and medical aids may lead to a break in provision of strongly co-dependent technologies, such as with insulin and SMBG. Many countries have taken action to overcome this hurdle, which requires a holistic view of the outcomes and costs in health care from the perspective of the entire society and not just from the perspective of a single payer.
Our study has some limitations. First, our search for full text articles was limited to one bibliographic database and was performed using a clinical trial identifier, which may have led to the loss of some relevant publications. Nevertheless, we were able to answer the primary question about the use of BG monitoring from the studies examined using a combination of sources, including full text articles, study synopses and EMA reports. The non-inclusion of existing full text reports may have potentially led to underreporting of dose adjustment, based on SMBG, and to the provision for training to patients on the use of SMBG. Second, our study scope was only on registered phase III studies, which was used as a foundation for insulin analog safety and efficacy claims and consequent regulatory approval, and did not include other pre- and post-marketing studies.
To conclude, the findings from this review endorse the crucial role of BG measurement in general and of SMBG specifically as a co-dependent intervention component of insulin treatment. The majority of phase III registration studies reported on the use of BG measurements for establishing safe and efficacious administration of insulin. The indispensable role of SMBG in treatment for insulin-dependent patients should receive the attention of health care payers in order to consistently assess and reimburse SMBG along with insulins to ensure the safety and effectiveness of insulin treatment.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Availability of data and materials.
All information, required to interpret results of the study is provided in the Tables 1 and 2 of the article.
Abbreviations
blood glucose
diabetes mellitus
European Medicines Agency
glycated hemoglobin
randomized controlled trials
standard deviation
self-monitoring of blood glucose
American Diabetes A. American. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37 Suppl 1:S14–80. doi: 10.2337/dc14-S014 .
Article Google Scholar
Scottish Intercollegiate Guidelines Network (SIGN). Management of diabetes. A national clinical guideline. Edinburgh (Scotland): Scottish Intercollegiate Guidelines Network (SIGN); 2010. Mar:170. (SIGN publication; no. 116).
Google Scholar
Working Group of the Clinical Practice Guideline on Diabetes Mellitus Type 1. Clinical practice guideline for diabetes mellitus type 1. Madrid (Spain): Basque Office for Health Technology Assessment, Osteba; 2012. May;1:345.
Medical Services Commission. Diabetes care. Victoria (BC): British Columbia Medical Services Commission; 2010. p. 17.
Rewers M, Pihoker C, Donaghue K, Hanas R, Swift P, Klingensmith GJ. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes. 2009;10 Suppl 12:71–81. doi: 10.1111/j.1399-5448.2009.00582.x .
Article PubMed Google Scholar
Medical Services Commission. Diabetes care. Victoria (BC): British Columbia Medical Services Commission; 2010. p.17. https://www.nice.org.uk/guidance/cg15 . Accessed 18 Dec 2013.
Caruso A, Hilsdorf HL, Mast O. Self-monitoring of blood glucose with insulin analogues: nice to have or need to have? analysis of phase III registration trials and european public assessment reports of insulin analogues. Value Health. 2013;16(7):A450. doi: 10.1016/j.jval.2013.08.731 .
Full reference: Canadian Optimal Medication Prescribing and Utilization Service.Optimal therapy recommendations for the prescribing and use of blood glucose test strips. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2009. https://www.cadth.ca/media/pdf/compus_BGTS_OT_Rec_e.pdf . Accessed 18 Dec 2013.
Washington State Health Care Authority. Glucose Monitoring: Selfmonitoring in individuals with insulin dependent diabetes, 18 years of age or under. Olympia (WA): Health Technology Assessment Program; 2011. http://www.hca.wa.gov/hta/documents/glucose_monitoring_final.pdf . Accessed 18 Dec 2013.
The SMBG International Working Group. Self-monitoring of blood glucose in type 2 diabetes: an inter-country comparison. Diabetes res clin pract. 2008;82(3):e17. doi: 10.1016/j.diabres.2008.08.021 .
Czupryniak L, Barkai L, Bolgarska S, Bronisz A, Broz J, Cypryk K, et al. Self-monitoring of blood glucose in diabetes: from evidence to clinical reality in central and eastern europe—recommendations from the international central-eastern european expert group. Diabetes Technol Ther. 2014;16(7):46–475. doi: 10.1089/dia.2013.0302 .
International Diabetes Federation Europe. Access to quality medicines and medical devices for diabetes care in Europe. 2013. http://www.idf.org/sites/default/files/FULL-STUDY.pdf . Accessed 18 December 2013.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of InterventionsVersion 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://handbook.cochrane.org . Accessed 18 Dec 2013.
European Medicines Agency (EMA). ICH Topic E 8 General Considerations for Clinical Trials. Note for guidance on general considerations for clinical trials (CPMP/ICH/291/95). 1998. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002877.pdf . Accessed 18 Dec 2013.
Weinzimer SA, Ternand C, Campbell H, Chang C-T, Becker DJ, Laffel LMB. A randomized trial comparing continuous subcutaneous insulin infusion of insulin aspart versus insulin lispro in children and adolescents with type 1 diabetes. Diabetes Care. 2007;31(2):210–5.
Garber AJ, Ligthelm R, Christiansen JS, Liebl A. Premixed insulin treatment for type 2 diabetes: analogue or human? Diabetes Obes Metab. 2007;9(5):630–9. doi: 10.1111/j.1463-1326.2006.00654.x .
Article CAS PubMed Google Scholar
Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Participants’ experiences of intensifying insulin therapy during the treating to target in type 2 diabetes (4-T) trial: qualitative interview study. Diabet med : j Br Diabet Assoc. 2011;28(5):543–8. doi: 10.1111/j.1464-5491.2010.03200.x .
Article CAS Google Scholar
Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, Keenan JF, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736–47. doi: 10.1056/NEJMoa0905479 .
Lindholm A, Jensen LB, Home PD, Raskin P, Boehm BO, Rastam J. Immune responses to insulin aspart and biphasic insulin aspart in people with type 1 and type 2 diabetes. Diabetes Care. 2002;25(5):876–82.
Pettitt DJ, Ospina P, Kolaczynski JW, Jovanovic L. Comparison of an insulin analog, insulin aspart, and regular human insulin with no insulin in gestational diabetes mellitus. Diabetes Care. 2003;26(1):183–6.
Moher D, Liberati A, Tetzlaff J, Altman D. The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 . Epub 2009 Jul 21.
Polonsky WH, Fisher L, Schikman CH, Hinnen DA, Parkin CG, Jelsovsky Z, et al. A structured self-monitoring of blood glucose approach in type 2 diabetes encourages more frequent, intensive, and effective physician interventions: results from the STeP study. Diabetes Technol Ther. 2011;13(8):797–802. doi: 10.1089/dia.2011.0073 .
Polonsky WH, Fisher L, Schikman CH, Hinnen DA, Parkin CG, Jelsovsky Z, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the structured testing program study. Diabetes Care. 2011;34(2):262–7. doi: 10.2337/dc10-1732 .
Article PubMed PubMed Central Google Scholar
Kato N, Cui J, Kato M. Structured self-monitoring of blood glucose reduces glycated hemoglobin in insulin-treated diabetes. J Diabetes Invest. 2013;4(5):450–3. doi: 10.1111/jdi.12072 .
Ceriello A, Barkai L, Christiansen JS, Czupryniak L, Gomis R, Harno K, et al. Diabetes as a case study of chronic disease management with a personalized approach: the role of a structured feedback loop. Diabetes Res Clin Pract. 2012;98(1):5–10. doi: 10.1016/j.diabres.2012.07.005 .
Mast O, Tan A, Zweyer A, Perridy D. Usage of self-monitoring of blood glucose (SMBG) by diabetes therapy type in larger cities in china. Value Health. 2012;15(7):A627.
Hermansen K, Fontaine P, Kukolja KK, Peterkova V, Leth G, Gall MA. Insulin analogues (insulin detemir and insulin aspart) versus traditional human insulins (NPH insulin and regular human insulin) in basal-bolus therapy for patients with type 1 diabetes. Diabetologia. 2004;47(4):622–9. doi: 10.1007/s00125-004-1365-z .
Degli Esposti L, Saragoni S, Blini V, Buda S. Effect of self-monitoring of blood glucose on glycemic control, clinical outcomes, and health care costs in diabetic patients using insulin: a retrospective analysis. Value Health. 2014;17:A323–686.
Mathieu C, Rodbard HW, Cariou B, Handelsman Y, Philis-Tsimikas A, Ocampo Francisco AM, et al. A comparison of adding liraglutide versus a single daily dose of insulin aspart to insulin degludec in subjects with type 2 diabetes (BEGIN: VICTOZA ADD-ON). Diabetes Obes Metab. 2014;16(7):636–44. doi: 10.1111/dom.12262 .
Weinzimer SA, Ternand C, Howard C, Chang C-T, Becker DJ, Laffel LMB, et al. A randomized trial comparing continuous subcutaneous insulin infusion of insulin aspart versus insulin lispro in children and adolescents with type 1 diabetes. Diabetes Care. 2008;31(2):210–5. doi: 10.2337/dc07-1378 .
Pettitt DJ, Ospina P, Howard C, Zisser H, Jovanovic L. Efficacy, safety and lack of immunogenicity of insulin aspart compared with regular human insulin for women with gestational diabetes mellitus. Diabet med : j Br Diabet Assoc. 2007;24(10):1129–35. doi: 10.1111/j.1464-5491.2007.02247.x .
Tamas G, Marre M, Astorga R, Dedov I, Jacobsen J, Lindholm A, et al. Glycaemic control in type 1 diabetic patients using optimised insulin aspart or human insulin in a randomised multinational study. Diabetes Res Clin Pract. 2001;54(2):105–14.
Home PD, Hallgren P, Usadel KH, Sane T, Faber J, Grill V, et al. Pre-meal insulin aspart compared with pre-meal soluble human insulin in type 1 diabetes. Diabetes Res Clin Pract. 2006;71(2):131–9. doi: 10.1016/j.diabres.2005.05.015 .
Bergenstal RM, Johnson M, Powers MA, Wynne A, Vlajnic A, Hollander P, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm with carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care. 2008;31(7):1305–10. doi: 10.2337/dc07-2137 .
Article CAS PubMed PubMed Central Google Scholar
Ratner R, Wynne A, Nakhle S, Brusco O, Vlajnic A, Rendell M. Influence of preprandial vs. Postprandial insulin glulisine on weight and glycaemic control in patients initiating basal-bolus regimen for type 2 diabetes: a multicenter, randomized, parallel, open-label study (NCT00135096). Diabetes Obes Metab. 2011;13(12):1142–8. doi: 10.1111/j.1463-1326.2011.01478.x .
Testa MA, Gill J, Su M, Turner RR, Blonde L, Simonson DC. Comparative effectiveness of basal-bolus versus premix analog insulin on glycemic variability and patient-centered outcomes during insulin intensification in type 1 and type 2 diabetes: a randomized, controlled, crossover trial. J Clin Endocrinol Metab. 2012;97(10):3504–14. doi: 10.1210/jc.2012-1763 .
Davidson MB, Raskin P, Tanenberg RJ, Vlajnic A, Hollander P. A stepwise approach to insulin therapy in patients with type 2 diabetes mellitus and basal insulin treatment failure. Endocr pract : off j Am Coll Endocrinol Am Assoc of Clin Endocrinologists. 2011;17(3):395–403. doi: 10.4158/ep10323.or .
Del Prato S, Nicolucci A, Lovagnini-Scher AC, Turco S, Leotta S, Vespasiani G. Telecare provides comparable efficacy to conventional self-monitored blood glucose in patients with type 2 diabetes titrating one injection of insulin glulisine-the ELEONOR study. Diabetes Technol Ther. 2012;14(2):175–82. doi: 10.1089/dia.2011.0163 .
Renard E, Dubois-Laforgue D, Guerci B. Non-inferiority of insulin glargine versus insulin detemir on blood glucose variability in type 1 diabetes patients: a multicenter, randomized, crossover study. Diabetes Technol Ther. 2011;13(12):1213–8. doi: 10.1089/dia.2011.0063 .
Kadowaki T, Nishida T, Kaku K. 28-week, randomized, multicenter, open-label, parallel-group phase III trial to investigate the efficacy and safety of biphasic insulin aspart 70 thrice-daily injections vs twice-daily injections of biphasic insulin aspart 30 in patients with type 2 diabetes. J diabetes invest. 2010;1(3):103–10. doi: 10.1111/j.2040-1124.2010.00015.x .
Cucinotta D, Smirnova O, Christiansen JS, Kanc K, le Devehat C, Wojciechowska M, et al. Three different premixed combinations of biphasic insulin aspart—comparison of the efficacy and safety in a randomized controlled clinical trial in subjects with type 2 diabetes. Diabetes Obes Metab. 2009;11(7):700–8. doi: 10.1111/j.1463-1326.2009.01035.x .
Bergenstal R, Lewin A, Bailey T, Chang D, Gylvin T, Roberts V. Efficacy and safety of biphasic insulin aspart 70/30 versus exenatide in subjects with type 2 diabetes failing to achieve glycemic control with metformin and a sulfonylurea. Curr Med Res Opin. 2009;25(1):65–75. doi: 10.1185/03007990802597951 .
Raskin P, Matfin G, Schwartz SL, Chaykin L, Chu PL, Braceras R, et al. Addition of biphasic insulin aspart 30 to optimized metformin and pioglitazone treatment of type 2 diabetes mellitus: the ACTION study (achieving control through insulin plus oral ageNts). Diabetes Obes Metab. 2009;11(1):27–32. doi: 10.1111/j.1463-1326.2007.00796.x .
Parkner T, Dyrskog SE, Laursen T, Chen JW, Mouritzen U, Brondsted L, et al. Obesity does not influence the unique pharmacological properties of different biphasic insulin aspart preparations in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12(5):414–20. doi: 10.1111/j.1463-1326.2009.01178.x .
Davidson JA, Liebl A, Christiansen JS, Fulcher G, Ligthelm RJ, Brown P, et al. Risk for nocturnal hypoglycemia with biphasic insulin aspart 30 compared with biphasic human insulin 30 in adults with type 2 diabetes mellitus: a meta-analysis. Clin Ther. 2009;31(8):1641–51. doi: 10.1016/j.clinthera.2009.08.011 .
Boehm BO, Home PD, Behrend C, Kamp NM, Lindholm A. Premixed insulin aspart 30 vs. Premixed human insulin 30/70 twice daily: a randomized trial in type 1 and type 2 diabetic patients. Diabet Med. 2002;19(5):393–9. doi: 10.1046/j.1464-5491.2002.00733.x .
Gao Y, Li G, Li Y, Guo X, Yuan G, Gong Q, et al. Postprandial blood glucose response to a standard test meal in insulin-requiring patients with diabetes treated with insulin lispro mix 50 or human insulin mix 50. Int J Clin Pract. 2008;62(9):1344–51. doi: 10.1111/j.1742-1241.2008.01850.x .
Download references
Acknowledgments
The study was supported by Roche Diabetes Care GmbH.
Author information
Authors and affiliations.
Synergus AB, Djursholmsvägen 20C, Danderyd, 18233, Sweden
Kaisa Miikkulainen, Rongrong Zhang & Oleg Borisenko
Roche Diabetes Care GmbH, Sandhofer Strasse 116, Mannheim, 68305, Germany
Antonio Caruso
Roche Diagnostics GmbH, Sandhofer Strasse 116, Mannheim, 68305, Germany
Oliver Mast
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Oleg Borisenko .
Additional information
Competing interests.
KM, RZ and OB are employees of Synergus AB, which received grant from Roche Diabetes Care GmbH, during the conduct of the study. AC is employee of Roche Diabetes Care GmbH. OM is employee of Roche Diagnostics GmbH.
Authors’ contributions
AC, OM and OB are the authors of general approach. KM and RZ participated in the systematic literature review. All authors participated in preparing, reading, and approving the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Miikkulainen, K., Caruso, A., Mast, O. et al. Systematic literature review of use of blood glucose monitoring in phase III clinical studies of insulin analogs. BMC Endocr Disord 16 , 21 (2016). https://doi.org/10.1186/s12902-016-0102-1
Download citation
Received : 15 November 2015
Accepted : 29 April 2016
Published : 04 May 2016
DOI : https://doi.org/10.1186/s12902-016-0102-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Blood glucose self-monitoring
- Diabetes mellitus
- Insulin analogues
- Phase III trials
BMC Endocrine Disorders
ISSN: 1472-6823
- General enquiries: [email protected]
A guide to writing your reflective report
A helpful guide for students wanting to complete a reflective report as part of their university accreditation. Updated October 2022
Find out more about delivering a local diabetes training programme

- Next Article
Reflections
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Irl B. Hirsch; Reflections. Clin Diabetes 1 October 2002; 20 (4): 162–164. https://doi.org/10.2337/diaclin.20.4.162
Download citation file:
- Ris (Zotero)
- Reference Manager
Looking into a mirror can be dangerous. On one hand, if the mirror is pointed straight ahead, the reflection could be an image that has gone through many changes. On the other hand, if the mirror is pointed at an angle, one can see images to the side or behind. It is with this in mind that we now turn toward our mirror at Clinical Diabetes.
This will be the last issue of the current editorial team. The 5-year term we complete here has coincided with what has probably been the most spectacular time in diabetes care since the discovery of insulin more than 80 years ago. In this issue, Dr. Arthur Krosnick provides an excellent rearview-mirror perspective on the history of diabetes care by chronicling his 47-year career as an endocrinologist ( p. 173 ). Dr. Krosnick’s article captures the essence of advances through the past five decades of diabetes treatment.
In the more recent past, much excitement in the field of diabetes during our editorial tenure has centered on new treatments. When this editorial team first met in the summer of 1997, insulin lispro (Humalog) had been released a year earlier, and it was already clear that this first insulin analog was a tremendous advance in insulin therapy. At that time, we were also writing our first prescriptions for thiazolidinediones, a new class of oral agents for the treatment of type 2 diabetes. Troglitazone (Rezulin) had just been approved for sale in the United States, and we were all excited about the potential role of this new insulin sensitizer.
Over time, of course, our enthusiasm waned as the first cases of severe hepatotoxicity were reported in 1998. Liver failure resulting in death or the need for liver transplantation made most of us much more cautious about troglitazone. Furthermore, many of us noted severe weight gain and even pulmonary edema resulting from its use with our patients. 1
Looking back, what was most disappointing to me was how so many in our field, including those marketing this drug, minimized these adverse effects. Many of us became quite upset and lost trust in the reassurances we had been given as adverse effects continued to be reported. Long after troglitazone was finally removed from the U.S. market in 2000, accounts in the popular press suggested that the situation had been even worse than we had suspected. 2
The silver lining in the troglitazone story is that it taught all of us to ask critical questions about subsequent new therapies. This is an important point, especially since we learned in 1998 that our older therapies were effective in reducing the microvascular and macrovascular complications of type 2 diabetes. 3 , 4 In this era in which “evidence-based medicine” is emphasized at every medical school in the country, 5 the United Kingdom Prospective Diabetes Study proved without question that our earlier therapies were both safe and effective.
It may well be that the newer therapies are even more effective than the older, proven treatments. But we need data on hard endpoints, both microvascular and macrovascular, before reaching such conclusions. As we have very recently learned through the Women’s Health Initiative regarding hormone replacement therapy, 6 it is difficult to draw definitive conclusions about our therapies until appropriately designed studies with clinically relevant endpoints are conducted.
Despite a wealth of data about the safety and effectiveness of insulin therapy, including for patients without diabetes hospitalized for myocardial infarction or after surgery, as a medical community, we continue to avoid the most important of all diabetes medications. One of the editorial team’s goals during the past 5 years was to make insulin therapy less intimidating to our primary care audience. This has become such an important issue for the American Diabetes Association that next year there will be a national clinical education program focused on the practical use of insulin therapy. Unfortunately, we hear all too often stories such as the one Ken Sanek tells in this issue ( p. 212 ) about type 2 diabetic patients whose providers remain resistant to insulin therapy.
Other advances in the past 5 years have included incredible improvements in everyday technologies for our patients. The size of glucose meters, the amount of blood they require, and the time necessary to complete the blood test have all improved.
Sophisticated data management systems for blood glucose readings are still underutilized but are now clearly gaining the interest of both doctors and patients. The trend is to use handheld devices to track glucose data; the ability to communicate this information to providers via the Internet is now a reality.
Insulin pumps have also improved, and we now have continuous glucose sensors as well. The Continuous Glucose Monitoring System was released in 2000, and earlier this year, the GlucoWatch became available. These first-generation devices will only improve with time.
In the past 5 years, we have also seen a real change in the epidemiology of type 2 diabetes, particularly in children. It is now estimated that type 2 diabetes accounts for 8–45% of pediatric patients with newly diagnosed diabetes in large U.S. pediatric centers. 7 These young patients are generally overweight with a strong family history of diabetes and often have other signs of insulin resistance.
Reflecting on what I believe to be the most important advance in the treatment of type 2 diabetes and macrovascular disease, I think of the numerous studies showing that pharmacological intervention can dramatically reduce the risk for cardiovascular events. The use of aspirin, angiotensin-converting enzyme inhibitors, and statins can reduce major events by 25, 25, and 30%, respectively. 8
Advances in our understanding of the prevention of diabetes have also generated tremendous excitement. The Diabetes Prevention Program proved that it is possible to delay the development of type 2 diabetes. 9 The Diabetes Prevention Trial–Type 1 (DPT-1), although a negative study, gives us further insight into how we may someday be able to prevent this challenging disease. 10 Incoming editor-in-chief Dr. Jennifer Marks discusses the implications of the DPT-1 in this issue’s “Landmark Studies” department ( p. 168 ).
The many changes in diabetes therapies have given us much to report in these pages. Our goal throughout this half-decade has been to bring advances in our understanding of diabetes, particularly diabetes therapies, to the primary care providers who see the majority of patients with diabetes. For this reason, we worked to ensure that our editorial advisory board included a large proportion of general internists and family practice physicians in addition to endocrinologists and members of the other health care disciplines involved in diabetes care. Working together, we were better able to meet our goal.
I would like to take this opportunity to thank our three associate editors who have worked extremely hard and made extraordinarily helpful contributions to the journal. Dr. William Herman, who served as an associate editor until this year, has taught me a great deal about evidence-based medicine and the science of the economics of medicine. Dr. Steven Edelman has become one of my best friends as well as my role model for how to be passionate about teaching physicians and patients about diabetes. Dr. Resa Levetan is perhaps the most creative physician I have ever met. Her ideas for developing interesting articles, translating new information to others, and getting physicians, patients, and their families involved with diabetes to obtain better outcomes are truly inspired.
I would also like to thank the many health care professionals who have served on our editorial board during these past 5 years, and especially Dr. Steven Leichter, who has written “The Business of Diabetes,” a department we added to our table of contents early on. Dr. Leichter’s provocative discourses on numerous topics in the world of finance and diabetes made this my favorite of the journal’s regular departments, and I am very appreciative of his efforts.
It is also important to acknowledge the assistance our team has received from the American Diabetes Association’s publications staff, particularly our publisher, Peter Banks; our managing editor, Aime Ballard; our assistant managing editor, Liz Rich; and the journal’s advertising and circulation staff. Most of all, the publication of Clinical Diabetes would not have been possible without the expertise of our project manager, Debbie Fentress.
Finally, I would like to thank all of the readers who have taken the time to write in with comments, both positive and negative, about our journal. Hopefully, we have succeeded in our mission to educate as many primary care providers as possible about state-of-the-art diabetes care.
It is time now to turn away from the mirror and to look forward. I have no doubt that the future of Clinical Diabetes will be even brighter than its present with Dr. Marks of the University of Miami in the editor’s chair. She and her team are already planning the first few issues of 2003. I am confident you will find the information they provide both interesting and relevant to your daily clinical practice.
Email alerts
- Insulin Therapy
- In Pursuit of Type 1 Diabetes Prevention
- Five Decades of Diabetes Patient Care: The Time of My Life
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Blood Glucose Measurement – OSCE Guide
- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE , Medicine , Surgery , Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Table of Contents
Suggest an improvement
- Hidden Post Title
- Hidden Post URL
- Hidden Post ID
- Type of issue * N/A Fix spelling/grammar issue Add or fix a link Add or fix an image Add more detail Improve the quality of the writing Fix a factual error
- Please provide as much detail as possible * You don't need to tell us which article this feedback relates to, as we automatically capture that information for you.
- Your Email (optional) This allows us to get in touch for more details if required.
- Which organ is responsible for pumping blood around the body? * Enter a five letter word in lowercase
- Email This field is for validation purposes and should be left unchanged.
This capillary blood glucose measurement guide provides a step-by-step approach to performing blood glucose measurement in an OSCE setting with an included video demonstration.
- Gather equipment
Gather the relevant equipment and place in a clean tray:
- Non-sterile gloves
- Blood glucose reader (a.k.a. glucometer): calibrate using calibration fluid if required.
- Spring-loaded lancet: to obtain the blood sample.
- Testing strips: make sure the expiry date is valid.

- Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role .
Confirm the patient’s name and date of birth .
Briefly explain what the procedure will involve using patient-friendly language: “Today I need to measure your blood glucose level, which involves taking a very small blood sample from your fingertip. You will experience a sharp scratch when I take the sample, but this should be very brief.”
Gain consent to proceed with blood glucose measurement.
Ask the patient if they have any pain before continuing with the clinical procedure.
Position the patient sitting comfortably on a chair .
- Measure the blood glucose
1. Ensure the patient’s finger is cleaned prior to measuring capillary blood glucose:
- It’s important that the skin over the site being tested has been cleaned, as substances on the skin can affect the accuracy of capillary blood glucose results (e.g. substances containing sugar).
- Ask the patient to wash their own hands or alternatively you can clean the site with an alcohol swab (70% isopropyl).
- Make sure the skin over the testing site has dried completely before performing capillary blood glucose measurement.
2. Turn on the capillary blood glucose monitor and ensure it is calibrated.
3. Load a test strip into the glucose monitor.
4. Don a pair of non-sterile gloves.
5. Pick up the lancet and carefully remove the protective cap.
6. Prick the side of the patient’s finger with the lancet and gently squeeze the finger from proximal to distal to produce a droplet of blood. Some guides advise cleaning away the first drop of blood, however, there is no evidence that this significantly impacts the reliability of blood glucose results.
7. Gently touch the tip of the test strip against the droplet of blood to allow it to be absorbed into the strip.
8. Apply gauze or cotton wool to the puncture site to stop the bleeding and ask the patient to maintain pressure over the site.
9. Safely dispose of the lancet into a sharps bin.
10. Dispose of the test strip and the cotton wool/gauze into a clinical waste bin. If the patient’s finger is still bleeding, keep the cotton wool or gauze in place and secure with some tape.
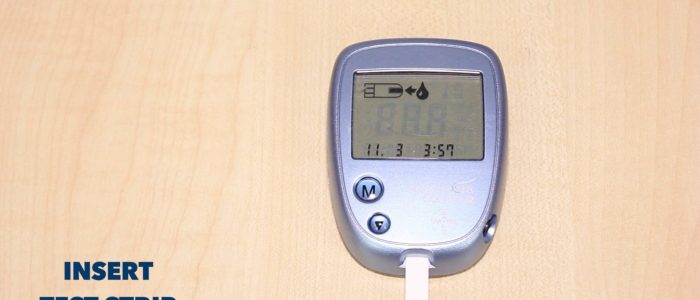
To complete the procedure…
Explain to the patient that the procedure is now complete .
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands .
Document the capillary blood glucose results on the appropriate chart.
Michelle Spence
Senior Nurse Practitioner

- Wash your hands and don PPE if appropriate
- Introduce yourself to the patient including your name and role
- Confirm the patient's name and date of birth
- Briefly explain what the procedure will involve using patient-friendly language
- Gain consent to proceed with blood glucose measurement
- Ask the patient if they have any pain before continuing with the clinical procedure
- Position the patient so that they are sitting comfortably on a chair
- Ensure the patient’s finger is cleaned prior to measuring capillary blood glucose
- Turn on the capillary blood glucose monitor and ensure it is calibrated
- Load a test strip into the glucose monitor
- Don a pair of non-sterile gloves
- Pick up the lancet and carefully remove the protective cap
- Prick the side of the patient’s finger with the lancet and gently squeeze the finger from proximal to distal to produce a droplet of blood
- Gently touch the tip of the test strip against the droplet of blood to allow it to be absorbed into the strip
- Apply gauze or cotton wool to the puncture site to stop the bleeding and ask the patient to maintain pressure over the site
- Safely dispose of the lancet into a sharps bin
- Dispose of the test strip and cotton wool/gauze into a clinical waste bin. If the patient’s finger is still bleeding, keep the cotton wool or gauze in place and secure with some tape.
- To complete the procedure…
- Explain to the patient that the procedure is now complete
- Thank the patient for their time
- Dispose of PPE appropriately and wash your hands
- Document the capillary blood glucose results on the appropriate chart

Other pages
- Product Bundles 🎉
- Join the Team 🙌
- Institutional Licence 📚
- OSCE Station Creator Tool 🩺
- Create and Share Flashcards 🗂️
- OSCE Group Chat 💬
- Newsletter 📰
- Advertise With Us
Join the community

IMAGES
COMMENTS
Blood glucose monitoring and management in acute stroke. care. Nursing Standard, 28 (19), 52-56. ... Clinical Placement Reflective Essay-final. Practice Nursing 92% (208) 4. Reflection Final - Assignment task 3. Integrating Practice 100% (9) 3. Using Gibbs Example of reflective writing in a healthcare assignment.
Appropriate and timely monitoring of blood glucose will allow for the successful management of blood glucose that is out of the target range. This will ensure ongoing patient safety during episodes of acute illness or effective management of diabetes mellitus in the longer term, minimising future diabetic-related health complications. Diabetes ...
within past 5 years; own functioning blood glucose meter and engage in blood glucose monitoring; and willingness to participate in the study by signing a consent form. Instruments Screening tools A demographic data collection tool and DM manage-ment education checklist designed specifically for this study and cognitive screening tool36 were used.
Similarly, no statistically significant result was found in self-care monitoring scores for the IG and CG over time using the SC-CII monitoring scale and SDSCA blood glucose and foot care subscales (P = .067, P = .67, and P = .638, respectively), although there was a trend toward higher self-care monitoring scores for the IG vs CG with the SC ...
The seven principles of effective self-care management include healthy diet, exercise, adherence to medication, glucose level monitoring, problem solving, reducing risks and healthy coping [ 5 ]. However, effectiveness of health education activities are affected by an individual's acceptance of their disease.
Blood glucose level is the amount of glucose (sugar) in the blood. It is also known as serum glucose level. The amount of glucose in the blood is expressed as millimoles per litre (mmol/l). Normally, blood glucose levels stay within narrow limits throughout the day (4 to 8mmol/l). But they are higher after meals and usually lowest in the morning.
The introduction of home blood glucose monitoring (BGM) in the late 1970s and regulatory clearance of the first meter for this purpose in 1980 revolutionized the self-care of people with diabetes (PWD) (1-3).Although often referred to as "self-monitoring of blood (or plasma) glucose," this form of glucose monitoring will be referred to by the more succinct "BGM" in this compendium.
Blood glucose monitoring is performed on patients with diabetes mellitus and other conditions that cause elevated blood sugar levels. Diabetes mellitus is a common medical condition that affects the body's ability to produce insulin in the pancreas and use insulin at the cellular level. There are two types of diabetes mellitus, type 1 and type 2.
The purpose of this study was to evaluate the effects of guided reflection on self-care behaviors, confidence scores, and diabetes knowledge among adults with diabetes. ... Informatively, IG critically analyzed 147 diabetes-related events concentrating on blood glucose, diet, exercise, monitoring, medication, sleep pattern, and health care ...
Please include the following details when submitting your typed reflective report as a word document: PITstop reflective report. Student PITstop ref number: Day 1 date of PITstop diabetes course: Submission date: Submit to [email protected]. Tips. You are expected to write a reflective report based on one of your insulin or ...
Blood glucose monitoring helps to identify patterns in the fluctuation of blood glucose (sugar) levels that occur in response to diet, exercise, medications, and pathological processes associated with blood glucose fluctuations, such as diabetes mellitus. Unusually high or low blood glucose levels can potentially lead to life-threatening conditions, both acute and chronic.
Physical activity and exercise play an important role in the prevention of complications and management of glucose in people with DM. 67-70 It is shown they can improve blood glucose control, reduce cardiovascular risk factors, improve well-being and assist in weight loss. 71-73 An exercise intervention of a period of eight weeks at least ...
The learning objective of comprehending the significance of blood glucose monitoring in diabetes management and mastering accurate monitoring techniques is essential for effective diabetes care. This reflection essay delves into whether the set objectives were achieved within the allocated time frame, offering insights into the experience and ...
Be able to appropriately monitor blood glucose levels in people with insulin-treated diabetes, if trained to do so. 5. Be able to competently inject insulin, if trained to do so. 6. Demonstrate an understanding of the right timing of insulin doses in common hospital scenarios. 7.
Introduction: Background. Self-monitoring of blood glucose (BG) levels is critical to the daily self-management for people with diabetes. In people with type 1 diabetes (T1D) the Diabetes Control and Complications Trial (DCCT) demonstrated that intensive insulin regimens and BG control corresponded with better glycemic control and resulted in a significant decrease in the macro- and ...
Blood glucose measurement has been highlighted for a diabetes treatment; it has been shown that effective monitoring of blood glucose can lead to 30-70% decrease in progression of the disease. (Diabetes control and complications trial research group, 1993) With careful administration, these complications can be delayed and even prevented.
Background Safe and effective insulin therapy for diabetes mellitus requires initial dose titration and regular adjustments based on blood glucose (BG) monitoring. Our objective was to explore the use of BG measurement in phase-III clinical studies of insulin analogs. These studies provide safety and efficacy information for regulatory authorities and are the basis for insulin analog ...
A guide to writing your reflective report; A summary of oral diabetes medications; Blood glucose strip calculator and DVLA monitoring requirements; Course evaluation example; Diabetes UK poster; PITstop GLP-1 care pathway; Grading criteria; Harvard reference guide; HbA1c chart; Illness algorithm; Insulin Care Pathway; Insulin profiles; Insulin ...
Decent Essays. 985 Words. 4 Pages. Open Document. eflective Account 3 : Blood glucose monitoring. Description. During my placement I was asked by my mentor to perform a blood glucose reading . The patient was a 78 year old gentleman Mr P with diabetes type 2. I have introduced myself , checked the patient's identity and asked for permission to ...
On one hand, if the mirror is pointed straight ahead, the reflection could be an image that has gone through many changes. On the other hand, if the mirror is pointed at an angle, one can see images to the side or behind. It is with this in mind that we now turn toward our mirror at Clinical Diabetes. This will be the last issue of the current ...
Glucose monitoring is done to obtain information on blood glucose levels to ensure a therapeutic regimen; the aim is to maintain consistent glucose levels and avoid hypoglycaemia and hyperglycaemia. Self-management is central to diabetes control. Diabetes is individual, so self-monitoring of blood glucose (SMBG) targets and frequency of testing must be decided to meet each patient's needs ...
3. Load a test strip into the glucose monitor. 4. Don a pair of non-sterile gloves. 5. Pick up the lancet and carefully remove the protective cap. 6. Prick the side of the patient's finger with the lancet and gently squeeze the finger from proximal to distal to produce a droplet of blood.